Medical Disclaimer: The information presented on this website is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be patient education, and does not create any patient-physician relationship.
ANS Dysfunction and Common Symptoms
AUTONOMIC FUNCTION AND DISEASE
There is a growing amount of scientific evidence telling us that one of the earliest triggers of chronic disease is dysfunction of the Autonomic Nervous System, and we can detect these changes before the onset of physical symptoms. A decrease in Parasympathetic branch functioning, and then malfunctions of the Sympathetic branch are the first steps in the development of such common diseases as diabetes, high blood pressure, fatty liver disease and heart disease.
Detecting and reversing parasympathetic and Sympathetic dysfunction is paramount to restoring your physiology and reversing the underlying process that fuels these common disorders. Short of this, modern medicines will only mask the cause of a person’s failing health.
Here are more common symptoms Autonomic dysfunction
Improving or restoring Autonomic function helps alleviate or reverses a wide array of problems.
See Hypohidrosis/Anhidrosis for lack of sweating, and Hyperhidrosis for excessive sweating.
Both sympathetic and parasympathetic branches are significantly damaged leading to an inadequate functioning at rest known as low HRV (heart rate variability). There are 2 levels of advanced autonomic damage.
The first is AAD (advanced autonomic dysfunction), also known as DAN (diabetic autonomic neuropathy) in diabetics. The most advance is CAN (cardiac autonomic neuropathy).
CAN carries 50% chance of death within 5 years from multiple causes including sudden death syndrome.
Insufficient or lack of sweating often on some parts of the body but not others. Skin may dry and crack in areas, and can be associated with heat intolerance. Often due to either decreased sympathetic activity and/or an excessive parasympathetic state.
A common form of anxiety is the result of a weak sympathetic response and results in inadequate blood and oxygen delivery upwards against gravity into brain. The body responds by releasing a surge of noradrenaline. This is often also associated with low HRV (heart rate variability).
An additional form of anxiety is from direct damage to the amygdala and results in an excessive sympathetic state.
If not a result of ischemia or congenital defect, arrhythmias are often secondary to autonomic imbalances of both the parasympathetic and sympathetic branches.
Parasympathetic damage contributes to the chronic inflammatory state that damages to the inner lining of blood vessels (endothelium).
Anesthesia suppresses autonomic function. If a patient with DAN or CAN may require lower doses of anesthetic medications.
The development of autism is being attributed to a neuroanatomical combination of propionic acid toxicity plus developmental delay (ineffective synaptic pruning and synaptogenesis from abnormal microglial functionality) plus delayed white matter of the emotional processing tracts. The damage from pro-inflammatory cytokines results in decreased sympathetic and parasympathetic function. The Nemechek Protocol improves microglia function, lowers inflammation, lowers propionic acid, and improves many symptoms associated with autism.
Increasing evidence suggest that many autoimmune disorders occur only after damage to the inflammatory neural circuit which contains both sympathetic and parasympathetic fibers.
Early autonomic dysfunction of Stage 1 (weak parasympathetic function on paced breathing and sympathetic excess on valsalva) and Stage 2 (sympathetic weakness and/or parasympathetic excess on valsalva) commonly occur without symptoms.
Symptoms begin to be felt in Stage 3 (sympathetic weakness or parasympathetic excess during a 5-minute test).
Stage 4 is associated with weak parasympathetic and/or sympathetic function are below normal during a 5-minute seated resting test. This is often referred to as low HRV (heart rate variability).
Stage 5 is an advanced state of autonomic weakness characterized by extreme parasympathetic weakness often with accompanying stronger sympathetic function, and is referred to as CAN (cardiac autonomic dysfunction).
Bipolar disorder is often accompanied by anxiety from sympathetic deficient or excessive responses as well as depression which is often associated with low HRV (heart rate variability) at rest but excessive parasympathetic responses on dynamic testing.
Dysfunction of both sympathetic and parasympathetic branches can result in urgency, retention, incontinence or frequent nighttime urination.
Broken Heart Syndrome is the result of sympathetic damage brought on by intense grief or fear. The damage results in a form of heart failure known as Takotsubo cardiomyopathy.
An extremely advanced state of autonomic weakness characterized by extreme parasympathetic weakness often with accompanying stronger sympathetic function (sympathovagal imbalance).
Autonomic Nervous System testing can provide early detection and intervention of cardiovascular disease: hypertension, cardiomyopathy, congestive heart failure, cardiac ischemia, coronary artery and heart disease, and cardiac dysrhythmias.
Cardiovascular disease is often accompanied by high sympathetic and low parasympathetic activity.
Unexplained arrhythmia, also called “heart palpitations”, may be reflection of an imbalance of both the sympathetic and parasympathetic branches.
This can occur from a variety of sources, many of which are associated with an imbalance of both the sympathetic and parasympathetic branches.
Chronic fatigue Syndrome is associated with deficient parasympathetic and sympathetic function at rest as well as low HRV (heart rate variability).
Sympathetic excess states may increase perception of tissue pain.
CRPS is associated with a combination of excessive parasympathetic and sympathetic function in the affected region or limb. The heightened sympathetic reactivity causes heightened sensitivity to pain.
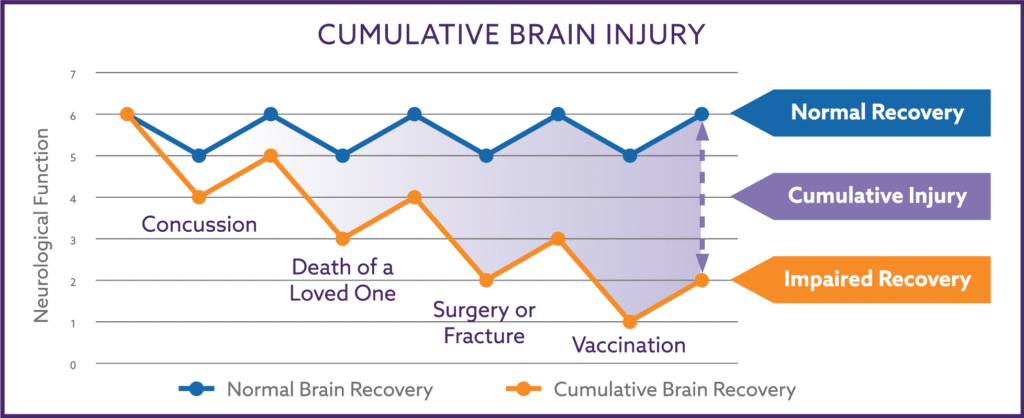
Although a physical trauma to the skull can damage any portion of the nervous system, the sympathetic branch is commonly injured and results in symptoms such as lightheadedness, headaches, anxiety, poor concentration or focus, and chronic fatigue.
COPD is associated with increased parasympathetic workload since the Vagus nerve must work harder to run ventilation.
Almost all diabetics develop progressive autonomic dysfunction over time, and it is recommended by the American Diabetes Association that all Type 2 Diabetics get autonomic testing within 2 years of diagnosis, and periodically thereafter.
The progressive nature of diabetes often results in premature deterioration of autonomic function up to 2 decades early.
DAN is associated with weak autonomic function at rest with weak parasympathetic function sometimes accompanied by weak sympathetic function.
In nondiabetics, the same level of weakness is referred to as Advanced Autonomic Dysfunction (AAD). Both AAD and DAN proceed the development of CAN.
This is often due to an inadequate sympathetic response when a person is upright and results in inadequate delivery of blood and oxygen to the brain.
Depression may be associated with weak parasympathetic function and low HRV (heart rate variability) while at rest but parasympathetic excess during dynamic testing.
Edema from venous insufficiency of the legs is due to sympathetic weakness while in the upright position.
Erectile dysfunction and vaginal lubrication are often due to weak parasympathetic function while the inability to ejaculate and orgasm may be due to weak sympathetic function.
This is due an inadequate supply of blood and oxygen to the brain and often due to inadequate sympathetic function while upright.
Daytime fatigue can be the result of parasympathetic excess or sympathetic weakness on dynamic resting, and both will contribute to low cerebral blood flow.
Fibromyalgia is often associated with weak parasympathetic function at rest with weak parasympathetic function and sympathetic function being noted on dynamic testing.
Gastroparesis is associated with weak parasympathetic function, and results in slowed peristalsis of the stomach (gastric) muscles.
GI distress is often due to parasympathetic dysfunction. The parasympathetic branch greatly influences intestinal motility.
The acid retention associated with GERD or heartburn is a consequence of the parasympathetic branch not emptying the stomach or controlling the lower gastroesophageal sphincter correctly. The parasympathetic branch greatly influences intestinal motility and function.
Depending on the cause, high blood pressure may be associated with sympathetic excess or withdrawal depending on the test performed.
Hyperhidrosis is excessive sweating often on some parts of the body but not others. Often due to excessive sympathetic activity.
Chronic low blood pressure is often due to sympathetic weakness or parasympathetic excess while upright.
Many headaches especially those that involve the rear of the skull (occiput) are the result of inadequate blood and oxygen delivery into the muscles of the scalp (known as coat hanger pain). These headaches are due to the inability of the sympathetic branch to counteract the forces of gravity, and results in the inadequate delivery of blood and oxygen to the tissues.
Insomnia can be the consequence of either sympathetic weakness while upright during the day or parasympathetic excess state during the night.
IBS is often due to parasympathetic dysfunction. The parasympathetic branch greatly influence intestinal motility.
This is often due to an inadequate sympathetic response when a person is upright and results in inadequate delivery of blood and oxygen to the brain. Can be accompanied by an excessive parasympathetic response when upright as well.
Migraine headaches are often associated with weak sympathetic function and excessive parasympathetic function on dynamic testing.
Since multiple sclerosis is an inflammatory disorder affect any portion of the nervous system, it is associated with a wide variety of autonomic patterns that all often result in low HRV (heart rate variability), AAD and CAN.
MSA is a progressive, neurodegenerative disorder of the autonomic nervous system and results in diffuse weakness of both sympathetic and parasympathetic branches.
Narcolepsy is associated with excessive parasympathetic responses on dynamic testing.
A common cause of chronic nausea is retention of stomach acid and may be a consequence of the parasympathetic branch not emptying the stomach correctly. The parasympathetic branch greatly influence intestinal motility and function.
Sympathetic weakness while in the upright position results in an increased level of thirst and hunger because blood flow to the brain is temporarily boosted by the intake of liquids and food contain salt and carbohydrates.
This is often due to an inadequate sympathetic response when a person is upright and results in inadequate delivery of blood and oxygen to the brain. Can be accompanied by an excessive parasympathetic response when upright as well.
Autonomic dysfunction can trigger increased levels of hunger resulting in the over-consumption of nutrients and calories leading to a pathological condition referred to as “overnutrition”. Overnutrition contributes to systemic inflammation, and results in cellular and organ damage including damage to the autonomic nervous system.
The sympathetic branch responds to injury and activates tissue repair mechanisms. Once the tissue is repaired, the parasympathetic branch suppresses the inflammatory repair process and returns the body to its normal resting state.
A weaken parasympathetic system often results in prolonged or exaggerated inflammatory responses, and is an important component for the activation of many autoimmune disorders.
Parkinson’s disease is a progressive neurodegenerative disorder often accompanied by a variety of autonomic features but often resulting in weakness of both sympathetic and parasympathetic function while at rest (low HRV).
The symptoms commonly associated with PMS are directly due to low brain oxygen delivery from the cerebral hypoperfusion caused weakness of the sympathetic branch. Prolonged menopausal symptoms often are from the same sympathetic dysfunction in addition to weakened parasympathetic functioning.
PTSD may be associated with weak parasympathetic function and low HRV (heart rate variability) while at rest but parasympathetic excess during dynamic testing.
Abnormal white matter track development in the sensory processing part of the brain. Similar to autism in that the brain is effected by propionic acid toxicity, plus developmental delay (ineffective synaptic pruning and synaptogenesis from abnormal microglial functionality), plus delayed white matter of the sensory processing tracks. This can be associated with decreased autonomic function and increases inflammation.
Sleep Apnea is associated with excessive parasympathetic responses on dynamic testing.
Insomnia can be the consequence of either sympathetic weakness while upright during the day or parasympathetic excess state during the night.
The normal regulation of sweating is primarily a function of the sympathetic branch.
This is due an inadequate supply of blood and oxygen to the brain and if often due to inadequate sympathetic function while upright.
This is often a normal compensatory response to low oxygen and blood pressure in the brain.
Broken Heart Syndrome is the result of sympathetic damage brought on by intense grief or fear. The damage results in a form of heart failure known as Takotsubo cardiomyopathy.
Although a physical trauma to the skull can damage any portion of the nervous system, the sympathetic branch is commonly injured and results in symptoms such as lightheadedness, headaches, anxiety, poor concentration or focus, and chronic fatigue.
Varicose veins of both legs is due to sympathetic weakness while in the upright position. Varicose veins of only one leg is often due to prior surgery, trauma or blood clots of the same leg.
True vertigo (spinning as if one were riding a carousel) is often due to dysfunction of the vestibule of the inner ear or sinus disease.
READY TO BOOK AN APPOINTMENT WITH DR. NEMECHEK?
Dr. Nemechek is a classically trained internist who is often able to quickly zero in on the cause of your symptoms though a simple question-answer session – a skill that is missing from modern medicine.
Educational Video Visits let people discuss with Dr. Nemechek about his protocol in detail. Only in-office appointments with Dr. Nemechek allow you to receive the full medical benefit of The Nemechek Protocol® medical consultation and treatment services.

Is Autonomic Dysfunction Affecting Your Health?
Take the Autonomic Health Quiz