Introduction
It is not uncommon for individuals to occasionally feel hungry, weak, and shaky or develop a ‘sour stomach’ between meals. Many will interpret this as a sign they need more nutrients because their symptoms seem to improve after they eat a little food. These symptoms can be so intense that it wakes them from their sleep.
Watch Dr. N’s CoffeeTalk on Heartburn
In spite of the fact these symptoms can improve with food, they have little to do with our biological need for nutrients or energy. You are about to learn that these symptoms are due to an abnormal buildup of stomach acid due to poor stomach and intestinal tract functioning.
How Does the Intestinal Tract Normally Function
Throughout the day, we constantly produce stomach acid. We produce even more when we eat a meal. Stomach acid is required to assist in digesting food, killing potentially harmful bacteria, and is also helpful in activating various digestive enzymes.
Think of your intestinal tract as a conveyor belt that constantly pushes your intestinal contents forward throughout the day. Our esophagus pushes food into the stomach, the stomach pushes stomach acid and partially digested food into the small intestine, the small intestine absorbs nutrients and pushes the non-absorbable material (fiber) into the colon, and the colon pushes material to the rectum.
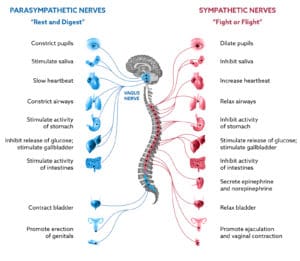
This conveyor belt action of the intestinal tract is primarily under the control of the neurological network referred to as the autonomic nervous system (ANS). The ANS is responsible for the contractions that empty the stomach and propel food along its course through the small and large intestines.
The conveyor belt action of the intestinal tract works 24 hours per day, emptying the stomach’s contents and passing it further along the way. When we eat food, the stomach is stimulated to produce even greater amounts of stomach acid and to empty even faster. This is an extremely important point because slowed emptying of the stomach triggers the single most common mimic of hunger, an excessive accumulation of stomach acid known as dyspepsia.
What’s the Difference Between Dyspepsia and Heartburn?
Heartburn occurs when the esophagus is exposed to stomach acid. The valve between the esophagus and the stomach is designed to allow food and liquid to pass downward from the esophagus into the stomach as well as to prevent the backwash of acid into the esophagus.
Occasionally, the valve relaxes, allowing stomach acid to reflux back into the esophagus. The acid stimulates nerve endings in the esophagus and causes the symptoms commonly referred to as heartburn or gastroesophageal reflux disease (GERD). GERD can be associated with a burning sensation in the chest, belching, a bitter taste in our mouth, coughing, and wheezing. Strangely, sometimes the refluxing acid will not cause any pain (referred to as silent reflux), can cause asthma after eating exacerbation, and trigger recurrent sinus and middle ear infections.
Dyspepsia is a term reserved for the symptoms we might think of as a sour stomach, slight nausea, or an upset stomach. These symptoms don’t result from acid splashing back into the esophagus as in heartburn. The symptoms of dyspepsia are from an abnormal accumulation of acid in the stomach. The acid accumulates because it is not being emptied normally, not because our stomach is producing too much.
To review, the symptoms of GERD are from stomach acid splashing back into the esophagus, and dyspepsia is from too much acid accumulating in the stomach.
Excess Stomach Acid Mimics Hunger
We often confuse dyspepsia with hunger because you may feel shaky, slightly nauseated, or weak, and eating food makes the symptoms disappear. They go away because food stimulates the stomach to empty. The food, therefore, causes the excess acid to be emptied into the small intestine, and your symptoms resolve.
The same symptoms will also go away if you take an antacid such as Tums since they result from excess stomach acid. But since they go away after you eat food, you draw the reasonable conclusion that the symptoms were due to low blood sugar levels or some other nutrient. Consequently, you believe your symptoms are a sign of hunger or “low blood sugar.” So the next time you feel similar symptoms, you’ll eat food again, and the symptoms go away again. After a while, it becomes almost second nature.
But why doesn’t the stomach work properly to empty the stomach acid in the first place? To understand why this happens, you’ll need to understand the autonomic nervous system.
Your Autonomic Nervous System
The autonomic nervous system is the portion of our brain that coordinates how our organs (heart, circulation, lungs, intestines, bladder, kidneys, and liver) function, how intensely we react emotionally, how our hormones are regulated, and how our immune system functions. Understanding if the autonomic system is functioning correctly is often the key to many medical puzzles.
The ANS is often referred to as the “automatic” nervous system in that its functions are not under voluntary control. And with such a major influence over the body, an imbalance in autonomic function is quite frequently a component of many chronic symptoms or illnesses.
Your autonomic nervous system may not always work correctly. A poorly functioning autonomic nervous system can be from damage to the nerves themselves, medications, and even from an imbalance of intestinal bacteria called SIBO, small intestine bacterial overgrowth.
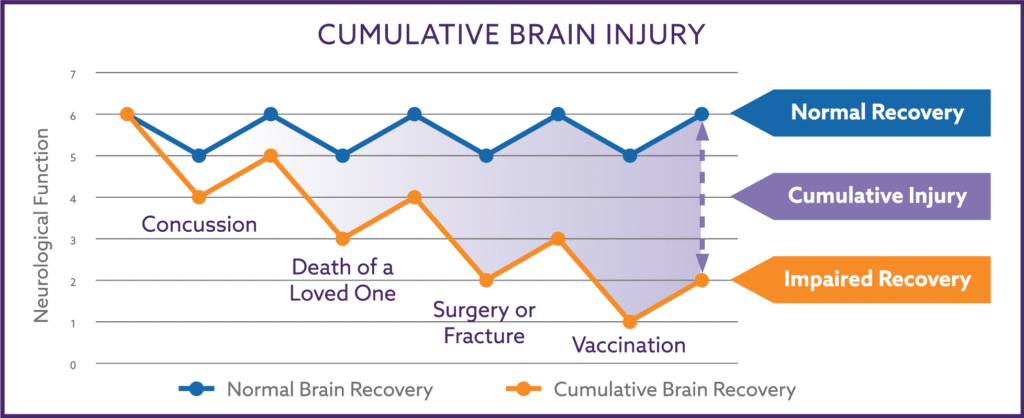
Damage to the autonomic nervous system can occur from physical traumas such as concussions, traumatic brain injuries, chemotherapy, radiation therapy, stroke, infections, or brain surgery. We now know autonomic damage can also occur from intensely negative emotional traumas.
The best-understood example is known as Takotsubo cardiomyopathy, the phenomenon otherwise known as “dying of a broken heart”. Intensely negative traumas such as the death of a loved one, molestation or rape, fear, divorce, and great financial loss all can damage the autonomic nervous system.
In addition to trauma, excessive consumption of nutrients such as omega-6 fatty acids (found in soy oil and other vegetable oils) or carbohydrates can lead to damage through a process known as overnutrition. Additional damage can occur through the “leaky gut” damage of bacterial overgrowth (SIBO), omega-3 fatty acid deficiency, and toxic exposure (chronic alcoholism, heavy metal exposure, pollutants).
Any of these conditions can subtly affect your autonomic nervous system causing your stomach not to empty correctly, giving you a sense of elevated hunger that is relieved by eating.
Heartburn and the Autonomic Nervous System
As discussed above, the Autonomic Nervous System (ANS) is a neurological network connecting your brain, spinal column, and nerves to every organ in your body. This connectivity allows the ANS helps regulate and coordinate the function of all your body’s organs.
The intestinal tract is primarily under the control of the parasympathetic branch of the ANS. The parasympathetic branch is primarily responsible for the contractions that empty the stomach and propel food along its course through the small and large intestines.
The ANS is particularly involved with the control and flow of the acid within our stomachs. The stomach is constantly producing acid throughout the day, and acid production is increased when we eat. When we swallow food, it passes through the esophagus down into the stomach. A valve between the esophagus and the stomach is meant to prevent acid from splashing back into the esophagus when the stomach begins contracting to digest our food.
While the stomach is contracting, the valve between the esophagus and the stomach needs to remain tightly closed. Otherwise, the acid can splash backward and cause the symptoms of burning, belching and bitter taste we associated with heartburn or GERD.
Scientific studies show that dysfunction of the parasympathetic branch of the ANS is the cause of poor esophagus-stomach valve function. Throughout your life, you’ve heard multiple medical explanations for heartburn, such as hiatal hernia, acidic foods, caffeine, alcohol, and being overweight. These reasons have either been proven incorrect (e.g., hiatal hernia), contribute to excessive acid production (e.g., large meals), have been discovered to contribute to the poor functioning of the autonomic nervous system (e.g., alcohol, caffeine), or worsen underlying small intestine bacterial overgrowth (SIBO).
Gut Bacteria and Heartburn
Your intestinal bacteria should be concentrated in the lower colon, with very few bacteria in the upper small intestine, where most nutrients are digested and absorbed. For every one bacteria in the upper small intestine, there are 100 million bacteria in the lower colon!
Unfortunately, some colon bacteria will find their way up into the upper small intestine (SIBO) and can trigger heartburn. This form of heartburn is often triggered by a particular type of food. Common examples are spicy food, tomatoes, lettuce, cucumbers, bell peppers, and certain fruit or nuts. Some estimates are that SIBO may affect 50-75% of the U.S. population.
If someone has abnormal bacteria in the upper intestine that are activated by nutrients found in spices, the active bacteria are capable of sending a signal up the vagus nerve ( a major nerve of the autonomic nervous system) and telling the brain to slow down the intestinal tract and not to empty the stomach. This happens with any kind of nutrient the bacteria are activated by.
If the stomach isn’t emptying while you are eating, the food contents and accompanying digestive enzymes and acids overfill. This will make you very bloated and cause the reflux of the overfilled stomach contents into the esophagus, giving you heartburn. The slowing of the intestinal tract is also responsible for your intestinal cramping and constipation, and if the overgrowth is bad enough, you develop diarrhea with particular foods.
Obesity, Insulin Resistance, and Carbohydrates
The increasing rate of obesity in the United States is associated with a growing incidence of insulin resistance. Insulin resistance is a metabolic disturbance that causes a wide variety of medical problems such as type 2 Diabetes, Hypertension, abnormal cholesterol, heart disease and strokes, Sleep Apnea, many forms of cancer, and Polycystic Ovarian Disease.
Insulin resistance was originally thought to be a consequence of obesity, but its cause seems to be more complicated than simply being overweight. Accumulating evidence suggests that insulin resistance is more the consequence of the chronic inflammation triggered by the type of foods we eat as well as inflammation released from body fat itself.
The reason weight loss helps with insulin resistance is that the levels of inflammation generally decrease with a loss of body fat, and a decrease in carbohydrates can reduce the degree of SIBO by starving off excessive bacteria within the small intestine. In a recent study that showed significant improvement in insulin resistance because of weight loss, the study participants had decreased their carbohydrate intake by about 100-150 grams per day. That’s a reduction of the average American’s carbohydrate intake by 1/3 to 1/2.
Many patients have successfully treated their symptoms from excess acid accumulation by simply reducing their carbohydrate intake. Most didn’t lose a significant amount of weight but still had significant improvement in their symptoms with carbohydrate reduction alone. Many were able to stop taking the antacids they had previously been prescribed.
Countless studies demonstrate the ability of weight loss to reverse diabetes, high blood pressure, and sleep apnea and reduce the risk of stroke, heart disease, and cancer. Again, these countless studies were seeing not only the sole beneficial effects of weight reduction per se but also the beneficial effects of reduced carbohydrate intake associated with the decreased caloric intake necessary for weight loss.
When viewed in this respect, it’s easy to understand why some individuals at a normal weight who eat a relatively high proportion of carbohydrates still can develop dyspepsia as well as disorders related to insulin resistance, such as high blood pressure, diabetes or heart disease.
Remember, it’s not really their weight that makes the difference; it’s the proportion of carbohydrates they eat, their age (we become more sensitive as we get older), and genetic differences in their sensitivity to the toxic nature of excessive carbohydrates.
How Do Carbohydrates Harm Our Autonomic Nervous System?
Excessive dietary carbohydrates can lead to an increase in metabolic inflammation in the brain through a process known as overnutrition. A variety of studies are demonstrating that metabolic inflammation can directly impair the functionality of the autonomic nervous system.
The negative autonomic impact of excessive carbohydrates helps explain why carbohydrate reduction improves many physical symptoms of autonomic dysfunction, such as urinary frequency, heartburn, bloating, and lightheadedness. Many researchers now believe that the high levels of carbohydrates in the typical American diet are in excess of a threshold that our modern brains can tolerate.
Another example of a food item that can cause toxic effects when consumed in excess is alcohol. Many studies have shown that drinking 1-2 alcoholic beverages, such as wine, per day is seemingly harmless to our health. But it’s commonly known that drinking 1-2 bottles of wine per day more than likely leads to poor brain health, damage to the liver known as cirrhosis as well as damage to our heart muscle (a condition known as cardiomyopathy).
Also, people falsely believe they needn’t worry about eating too many carbohydrates if they exercise regularly. They will simply “burn them off.” The toxicity of excessive carbohydrates is not due to the excessive calories they may provide but more due to the toxic effect.
You Can’t Outrun a Bad Diet
Thinking that exercise can rid one of the toxic effects of carbohydrates is similar to alcoholics thinking that drinking a bottle of vodka is harmless since they will exercise enough to burn off the calories in the vodka. Exercising more may burn off more calories but will not affect the potentially toxic nature of an excessive intake of alcohol or carbohydrates.
The amount of carbohydrates in the American diet over has crossed a toxicity threshold in many individuals. The toxicity of excessive carbohydrate consumption is resulting not only in the diseases associated with insulin resistance but is also damaging our autonomic nervous system.
Remember, the autonomic nervous system controls the function of every organ in your body. And when the autonomic system is damaged and not functioning properly, we experience symptoms such as bloating, heartburn, lightheadedness, fatigue, excessive sweating, flushing of our skin, constipation, urinary frequency, and urgency, and incontinence.
Reduce your carbohydrate intake, and you can eliminate these symptoms.
How Many Carbohydrates Should We Eat?
To answer this question, we need to look at the evolution of our Stone Age ancestors and the amount of carbohydrates they consumed. Scientific evidence suggests that our primitive ancestors ate a diet that consisted predominantly of animal tissue (protein and fat) and plants known as browsing foliage (dark green leafy plants).
During the Stone Age, carbohydrates were very uncommon in the wild and consisted of occasional roots, wild fruit, or honey. Overall, the availability of carbohydrates was uncommon. Other than being on a tropical island, when was the last time you saw some fruit, such as an apple or orange, when walking in the woods? These foods do not grow commonly in the wild. They are cultivated plants that became more readily available after the agricultural revolution.
Many Americans consume more carbohydrates per day than our Stone Age ancestors consumed in a year. The amounts of carbohydrates available for human consumption didn’t begin to increase until the agricultural revolution (5,000 -10,000 years ago) when man learned to grow grains such as wheat, barley, and millet. The domestication of livestock and the consumption of livestock milk became an additional source of carbohydrates (milk sugars) as well.
But 10,000 years is a very small span of time from an evolutionary perspective. Although there may have been a few beneficial evolutionary mutations associated with protection from infectious diseases in the last 10,000 years, science has failed to demonstrate any adaptive genetic mutations that might have changed with the subsequent marked increase in carbohydrates in the human diet.
To put the evolutionary time span into perspective, if the entire span of human evolution is represented by a 100-yard football field, the last 10,000 years will encompass only the final ¼ inch of the entire 100-yard field. As you can see, 10,000 years is not significant compared to the millions of years required for human evolution.
The point of this is to help you understand that we were designed through evolution to adapt to eating predominantly animal tissue (protein and fat) and low amounts of carbohydrates. We did not develop the metabolic ability to handle such large quantities of carbohydrates in our diet, and our bodies are suffering because of it.
To put it another way, the average American consumes more carbohydrates in a day than our Stone Age ancestors consumed in a year. It’s the excessive amount of carbohydrates in our diet that are having a toxic effect on our nervous system.
Carbohydrate Reduction and the Theory of Neuroplasticity
Neuroplasticity is a relatively new scientific concept that our neurological tissues (brains, spine, and nerves) have some ability to recover function from at least mild levels of insult or damage. Neuroplasticity means ‘nervous tissue’ that has the ability to ‘regain its function’ after being altered, just as plastic regains its shape after being bent.
After a stroke, patients have the ability to regain some neurological function. After a nerve or the spinal column is damaged by an injury, remarkable degrees of recovery have been known to occur. The recovery in these cases may not be complete in severe cases but can often be complete with mild injuries to the nervous system.
After the Autonomic Nervous System (ANS) is damaged, it, too, shows a remarkable ability to recover from the toxic effects of excessive carbohydrates. Many patients have completely recovered from the neurological damage that causes heartburn, erectile dysfunction, lightheadedness, and urinary disturbances after reducing their carbohydrate intake.
One exception to the neuroplasticity of the ANS is in patients with long-standing type 2 Diabetes Mellitus. In this circumstance, the nerves have been severely damaged by the toxic effects of excessively high blood sugar and insulin levels as well as the damaging effects of inflammation associated with insulin resistance. Fortunately, most patients who have worked at controlling their diabetes still have a good chance of reversing their ANS dysfunction.
How Many Carbohydrates Are Too Much?
What should you reduce your total daily carbohydrate intake to? The average American diet now consists of 50-60% of calories from carbohydrates. Scientific studies suggest that you can greatly improve your health if you reduce your carbohydrate intake to approximately 20-25% of your total daily caloric intake. This is equal to about 100-125 grams of carbohydrates per day for women and 125-150 grams per day for men.
First, start by reducing the larger amounts of carbohydrates in your diet; start with frequent servings of potatoes, rice, pasta, and sugar-containing drinks. Replace these with more protein and low-carbohydrate vegetables.
After a week or 2, count the grams of the remaining carbohydrates in your daily diet for a few days. You will quickly realize the high amount of carbohydrates you have been consuming on a regular basis.
Reducing your carbohydrate intake to 20-25% of your total caloric intake has a dramatic improvement in the diseases arising from insulin resistance as well as improving your neurological functioning. Your triglyceride and HDL cholesterol levels will improve, your blood pressure will be greatly reduced, and your blood sugar levels will normalize as your body’s response to insulin improves.
Carbohydrate reduction has been calculated to have 6-8 times greater power of reducing the risk of cardiovascular disease (strokes and heart attacks) than do the statin medications that are commonly prescribed to lower LDL cholesterol levels. Why treat these conditions with potentially toxic medications when you can prevent and even reverse these conditions by simply reducing your carbohydrate intake?
Summary
If you’re experiencing persistent hunger between meals, occasional nausea or episodes that feel like low blood sugar, eliminate these symptoms by simply reducing the carbohydrates in your diet. You’ll notice a significant improvement in only a few weeks.
And if you have learned something useful from this article, I urge you to pass it on to 1 or 2 of your friends and encourage them to improve not only their lightheadedness and fatigue but their overall health as well.
Subscribe to Dr. N’s Health Thru Nutrition Blog


This is completely opposite to the article,
But can be food aversions a symptom of autonomic dysfunction too?
Possibly.
Hello Dr. N,
I appreciated your article and am hoping for input on my 10 year vegan diet. I consume vegs, legumes, and fruit; very little grain. Seldom consume bread. Is fruit harmful to the autonomic nervous system? Thank you,
Gem
No it is not
Hi! Last Wednesday night, I ingested a kitchen spoon of white vinegar to try and settle a stomach, but after swallowing I realized it was 25% vinegar essence(!), essentially super concentrated vinegar. Not good. After reading online I drank a lot of water and made myself vomit a couple times. After that, and a visit from the paramedics who said I had nothing to worry about, I went to sleep. The last few days I’ve heen having symptoms like you’ve mentioned above. A bit of burning in the esophagus and a hunger that shows up pretty soon after eating. My… Read more »
The gut is very resilient, and I think you’ll be back to baseline soon.
But if things worsen, seek medical care even while in Japan. They have an excellent medical system there.
Hi,
Every time I get (when I can – I have nausea everyday especially in the morning) my stomach always grumbles, it’s constantly burning & my appetite is really poor… I also get dizzy when I eat..
Is this SIBO? Or something else?
Possibly SIBO combined with some secondary autonomic dysfunction
Many thanks doctor for your reply on my previous comment. I did take xifaxan couple of times for SIBO as prescribed by my GI but dyspepsia symptoms
( constant hunger every 2 hours and belching ) still persist.
Then your remaining symptoms are from underlying autonomic dysfunction
Hello Dr, I am hoping you can throw some light on my misery. I was having constant hunger, heart burn, heavy belching and bloating before and after meals. . My current Gi doctor done endoscopy, 48 hour ph bravo test , res tech test, breath test for sibo. He found no acid reflux and endoscopy is also fine. But breath test is positive for hydrogen dominant Sibo. He told me that he found no acid in my stomach when he did endoscopy and thinks that all my problems are due to low stomach acid. Note that I was taking ppis… Read more »
I’d focus on reversing the SIBO
I am so grateful to have found your site and to you for taking the time to answer my questions and for the time it must have taken you to have such an understanding of these types of problems. In only a few days I was able to discontinue using omeprazole after about 2 years of taking it by using inulin twice a day and reducing carbs. to less than 100 grams/day. I haven’t felt this normal in a very long time! Thank you so much! I cannot wait for your protocol book to be available!
Your very welcome.
Hi Dr N
I am a 20 yrs old female and recently I’ve been experiencing hunger pain even after full meal like half an hour later and now pain isn’t subsiding even after eating. I was feeling dizziness like three days ago and when I checked up my Random blood sugar it was 53 mg/dl
A week ago I’ve been taking medicine for fungal infection (tinea interdigitale) itraconazole I thought that may be it could be side effects of drugs and now doctor has given me terbinafine.
So is it due to drugs or excess acid????
Plzz help me
I’m sorry I can’t answer such a specific question on a blog.
Is it possible to reverse SIBO without Xifaxan if I use inulin and reduce carbs. to less than 100 g?
Inulin in an adult surely can help with some of the symptoms but I have very little success in reversing chronic brain injury in adults over 35 years of age without inulin.
I am wondering if I should see a GI specialist or if this will turn into many tests that don’t provide answers, I wish you were closer! I was dx. with a stomach ulcer a few years ago. This was based on my symptoms and that omeprazole twice a day helped. I didn’t have any scope tests done and don’t want to due to fear of the scopes being properly cleaned. I was told that I would have to take the omeprazole for the rest of my life which seemed odd being I thought the ulcer would heal at some… Read more »
Could be bacterial overgrowth (SIBO) and if so would require Xifaxan to recover from.
In lieu of Xifaxan, I recommend my patients try inulin fiber as this can help the symptoms quite a bit. If it does, I interpret it to mean the patient has SIBO.
If it doesn’t, go t=see the GI doc to be certain it is not something worse.
Can you r protocol reverse autonomic nerve damage done by Levaquin, a fluoroquinolone antibiotic?
Maybe. I’ve never had the opportunity to reverse Levaquin neuropathy before.
Hi Dr. Nemechek, my daughter 8 yrs old has a diagnosis of ASD. We did the nemechek protocol of antibiotics for SIBO which made a positive change in her interaction, awareness and learning. But the omega 3 fishies are causing nausea and the inulin is constipating her.
I wonder if she has autonomic nervous system dysfunction. Whenever she is scared of something ( swimming pool or a dental appointment) she immediately gets a bowel movement. What should I do??
Fish oil and restoration of intestinal balance are essential for The Nemechek Protocol to work.
Read our book at https://autonomicrecovery.shop for all the details about what to do.
Hi Dr N, I’ve been struggling on and off with heart burn and indigestion to which I’ve visited a doctor a number of times, each time I have been prescribed Omoeprozole. I have found that in the past 12 months I have gained weight and am unable to lose it no matter how hard I try. I’ve attempted gluten and dairy free diets but still find I have reflux the majority of the day. This week I was prescribed Erythromycin for a tooth ache which has made the indigestion unbearable, I could not sleep last night due to acid regurgitation… Read more »
Look into rebalancing your gut with some inulin fiber. Read my article on SIBO and the most recent article on Probiotics.
Hi Dr. N
Thanks for your informative article.
I have the symptoms of excess stomach acid with the aching “need to eat” about 1 1/2 hours after I eat. I have cut out ALL dairy, wheat, fruit and high starch vegetables like potatoes in the last 2 weeks. I also have persistent insomnia anytime after 1Am, often not being able to return to sleep. I am at a loss to know where to turn. My Dr gave me Tecta, but I am reluctant to take it. What would you suggest?
Thanks so much
After eating an average sized meal, an adult will shunt about 30% of all their blood volume from the peripheral circulation (that supports blood pressure to the brain) to the intestinal/mesenteric vasculature. This sudden drop in peripheral volume can result in a drop of brain blood and oxygen delivery. In my experience, this is one of the most common reasons people feel tired, lightheaded or hungry after eating, and is a sign of dysfunction of the autonomic nervous systems ability to compensate and maintain normal brain blood and oxygen delivery. In effort to normalize brain oxygen delivery, the brain increases… Read more »
I am on raniditine and it does work. I am 86 and frankly fed up with this problem. My
Gastro Doc thinks I might have micro colitis. This might be all connected.
Very interesting article I have GERD and a hiatal hernia. I always have an empty feeling in my stomach. Never realized carbohydrates were the cause. I usually try to eat more carbohydrates to eliminate the empty hungry feeling. I also experience light handedness. I am going to watch my carb in take and see if that helps. Thanks for the information!
Watch out. With the lightheadedness, it sounds like you are having some autonomic difficulties as the source of your GERD and lightheaded symptoms.
Cutting carbs can make the lightheadedness worse. Read my posts on Brain Fog
I came across your article while researching the stomach issues I’ve been experiencing. For the past week, when I start to feel hungry and get that hunger pang in my stomach, it’s been feeling a bit painful. I have always dealt with acid reflux and would deal with chest tightness because of it but I do not like taking medication for it and just try to avoid foods that trigger heartburn for me (cooked bell peppers). Could I be dealing with excess acid in my stomach? I currently take supplements as I have been trying to conceive for two years.… Read more »
Could be. Yes, go get checked out.
Dear Doctor N. I am a 73 year old male, I have suffered from stomach acid for the last 30 years, I wa on one medication or another to try to control it, there are so many confusing articles on the web that it’s hard to know what to believe, one doctor had me on Lozac for 5 years, I ended up with breast enlargement, another doctor had me on a medication not even covered by Ohip, at a cost of $400.00 every 3 months, a lot of information tells you that the symptoms are actually caused by not enough… Read more »
The symptoms from Heartburn or GERD are predominantly from normal acid production but excess acid retention in the stomach, not excessive production of acid. The retention is because the stomach does not empty the stomach correctly. It’s similar to when the kitchen sink overflows on the flow. Its not that the faucet if dumping too much water into the sink. Its because the sink can’t empty it. Apple cider vinegar could make you feel better because it lowers the pH (more acidic) but it could also make you feel better because you’re feeding the bacteria and cells that line the… Read more »
I like this article. I to seeing more of related articles’
Look around. There are plenty of articles that touch on the similar topic.
Hello i have been having major stomach issues for 1 year now, it started after 4 days of taking ibuprofen (600 mg) a day, that was advised to me by a docter because of a over encumbered wrist, the stomach pain i then got was horrible it felt like i had digested a Burning knife, and some rocks, i was then advised to take omeprazol for 4 weeks that did nothing, now one year further i fixed the bloating with probiotics, but im still experiencing pain all the time which gets worse on an empty stomach, should i take ranitidine… Read more »
If probiotics help you, you have SIBO. You need to focus on that.
Dr. N