Five Sources of Anxiety
Ever feel anxious but do not know why? A hormone called noradrenaline causes nervousness, a rapid heart rate, a sense of insecurity, and a feeling of fear that may be triggered in several different ways.
Understanding the different sources of anxiety may help people find the treatment answers that are best for each circumstance.
They all result in the release of noradrenaline so the physical reaction to each kind of anxiety is identical.
The first source of anxiety is when someone is confronted with a real and immediate danger. Noradrenaline is released in situations that are true threats to our survival, like being tied to the railroad tracks when there is an oncoming train.
This source of anxiety is a survival mechanism causing us to react to real danger in our presence.
The second source of anxiety may occur in situations when someone perceives that they are in danger and their body releases noradrenaline but they are, in fact, safe.
This is a kind of anxiety that psychologists and psychiatrists may help someone understand and work through to change their response to those situations. An unfounded fear of birds might be an example of this.
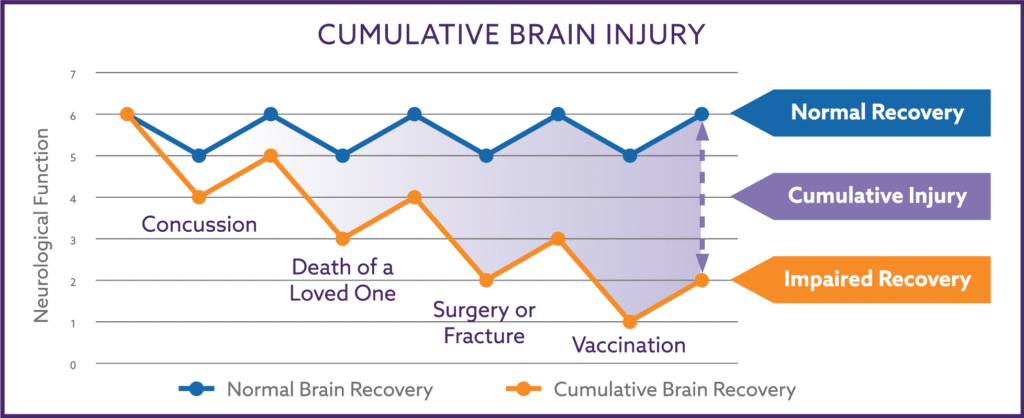
The third source of abnormal anxiety comes from direct damage to cells within the portion of the brain that normally regulates anxiety, the amygdala. The amygdala can be damage in physical injuries to the skull such as car accidents, falls, or the concussive blast that is associated with explosives.
The amygdala may also be damaged from intense emotional experiences and is a necessary component in the development of post-traumatic stress disorder (PTSD). Some relief may be found in low doses of Acetyl L-Carnitine, an over-the-counter supplement that increases the production of reparative stem cells in the brain.
The fourth source of abnormal anxiety comes from an imbalance of intestinal bacteria called Small Intestine Bacterial Overgrowth (SIBO). Our own gut bacteria migrate into the wrong section of our intestines.
This may occur when something alters the speed of our digestive tract such as antacids, antibiotics, anesthesia, vaccines, or as a result of Autonomic Nervous System Dysfunction (Dysautonomia).
SIBO is a condition that is estimated to affect up to 75% of the population but many people with SIBO report no intestinal symptoms. Others with SIBO experience intestinal distress (diarrhea, constipation, eat-and-must-go to the bathroom ASAP, excessive bloating), food sensitivities/intolerance, night sweats, morning nausea, sour stomach or “low blood sugar” between meals, skin problems (rashes, hives, eczema), and recurrent strep and bladder infections.
Intestinal bacteria alter how the nervous system functions through five different pathways and is also capable of triggering the release of anxiety-provoking noradrenaline.
SIBO is the major cause of anxiety when someone has a “nervous stomach”. Many of us have had intestinal symptoms before an anxiety-producing event such as public speaking or getting on an airplane.
The phrase “nervous stomach” implies the stress of the situation causes anxiety which in turn causes diarrhea. But studies suggest that the opposite is happening; the stressful situation alters the gut bacteria, and the bacteria trigger the release of norepinephrine leading to anxiety.
In other words, one experiences a “stomach nervous” instead of a “nervous stomach”. SIBO-driven anxiety is reversible in adults with a short course of medication called rifaximin and is reversible in kids with an OTC pre-biotic fiber called Inulin that one may buy from a variety of manufacturers in both powder or gummy forms.
The fifth source of abnormal anxiety is a mechanical problem leading to the inadequate flow of oxygen and blood flow into the brain when sitting or standing upright. This is a gravitational problem and is the consequence of Autonomic Nervous System Dysfunction.
Two quick tests for this type of anxiety are to see if the anxiety feelings improve after laying flat for 10 to 15 minutes, or after exercising. If the answer is yes to either, Autonomic Nervous System Dysfunction might be a source of the anxiety.
True anxiety stressors, like not enough money to pay bills or family holiday fights, do not improve when laying down or during exercise. Fortunately, anxiety from Autonomic Dysfunction can be diagnosed in a doctor’s office and reversed without long-term prescriptions.
The Autonomic Nervous System is how the brain controls and coordinates the function of the entire body though a system comprised of nerve impulses, hormone surges, and cellular responses.
This includes the brain’s ability to control heart rate, blood pressure, produce stress hormones, and maintain perfect cerebral blow flood upwards to the brain against gravity no matter what the body is doing.
The Autonomics may be injured and not function correctly after a (1) physical injury (concussion, car wreck, childbirth), (2) emotional event (an emotionally traumatic event, bullying, loss of a loved one), (3) metabolic or inflammatory event (excessive vaccine reaction, chemotherapy, radiation, heat stroke), or (4) by SIBO that interferes with Autonomic function.
The brain has about a one second supply of reserve oxygen, and it panics if the Autonomic Nervous System is not able to deliver the perfect flow of blood and oxygen upwards against gravity.
The primitive brain perceives the inadequate delivery of oxygen as a lethal threat, and does whatever is necessary to normalize the delivery of oxygen, including producing noradrenaline.
When someone lays down flat or does exercise, they give their brain a temporary boost of blood and oxygen, and they feel less anxious because the brain is no longer starving for oxygen.
A temporary boost of blood and oxygen may also come from eating salt, carbohydrates, or sugars that trick us into a false diagnosis of “low blood sugar” or feeling the irresistible need to snack between meals.
Another temporary boost comes from consuming sodas or other high carb/sugary drinks, foot tapping and leg bouncing, or smoking nicotine. Some people’s chronic hunger or thirst, hyperactivity, or nicotine addictions may just be an unconscious reaction to an unresolved Autonomic injury.
There are five stages in Autonomic Dysfunction and the first two stages do not have noticeable symptoms. It is only in the third stage of Autonomic Dysfunction that people start to experience symptoms that affect their daily life like anxiety, GI trouble, sleep trouble, headaches, temperature regulation problems, or dizziness.
Early Autonomic Dysfunction detection gives patients the opportunity to reverse the damage and prevent future complications such as headaches, chronic fatigue, high blood pressure, diabetes, or depression.
In patients already experiencing symptoms of Autonomic Dysfunction or who have already been diagnosed with a chronic disease, regular Autonomic or HRV monitoring helps measure their recovery, lowers their risk of premature death, improves their response to therapies or situations when the Autonomics are artificially suppressed (while under anesthesia), and helps get them off medications that mask their symptoms but do nothing to improve their health.
Autonomic Dysfunction does not appear on an MRI, CT scans, and it is not detected in yearly bloodwork. For over 10 years I have tested the Autonomics using spectral analysis to pinpoint the tone and balance of each of the Autonomic Nervous System’s two main branches, the Sympathetic (“fight or flight”) and the Parasympathetic (“rest and digest”). I also use Heart Rate Variability (HRV) testing as a marker for Autonomic function and recovery.
Groundbreaking bioelectrical work is now being done within the field of Autonomics and the stimulation of the Vagus Nerve that I believe will completely transform modern medicine and make many prescriptions obsolete in our lifetime.
I am an internal medicine physician (D.O.) from UCLA and my Internal Medicine and Autonomic practice is in the Phoenix area. I have discovered a multifaceted formula for Autonomic Nervous System restoration that is so groundbreaking that I was granted a patent for The Nemechek Protocol for Autonomic Recovery (Patent No. 10,335,396) in July 2019. For additional information, call my office 623-208-4226 or go to AutonomicMed.com.
I use all available scientific and medical tools to induce the nervous system and organs to repair themselves by normalizing inflammation control mechanisms, inducing natural stem cell production, and re-activating innate restorative mechanisms.
Fixing the brain, to fix the body, takes persistent effort by the patient but I have seen Autonomic injuries and anxiety recover years or decades after the person’s trauma or event. This is where hope can be found because it is never too late to improve one’s health.
If you or someone you know experiences abnormal anxiety, be aware that the Autonomics, SIBO, or damaged neurons may be to blame for the noradrenaline. Understanding that anxiety may be a mechanical, bacterial, or cellular damage issue may help people finally find the treatment modality that addresses their specific type.
Thankfully there are both traditional medications and naturally based solutions for all three types of abnormal anxiety.
© 2016. Dr. Patrick M. Nemechek and Jean R. Nemechek. All Rights Reserved. Patent Pending.
5
2
votes
Article Rating
Hello Dr N, My daughter will turn 5 next month. She is on a modified protocol from Feb 2019. and on the full protocol from April 2019. There are many gains that we observe like better eye contact, awareness, imitating and many more. But with gains, her behaviour gets more aggressive as well. from June last 1 month, she starts hitting herself(slapping her head). even her teachers complain that she hit herself so hard. please guide.
Doses:
1/8 tsp inulin
Nordic Natural Omega 3- 2.5ml
Evoo-5ml
The increasing aggressive behaviors is often from decreasing brain BP. The summer heat can cause this as can another injury.
Try increasing her salt and water intake.
I have had chronic IBS-C for close to 30 years, mostly presenting itself mostly as bloating / burping and incomplete evacuation. I had a panic attack in 2010 that lasted for a week but has not recurred. In 2017, I quit smoking (started around the same time as the IBS), which after a couple of months caused a flare up of IBS, waking me up 90 minutes into sleep and then the burping would keep me from sleeping. This caused a lot of sleep anxiety and a weight loss of 20lbs in a month, and was prescribed 7.5mg remeron. My… Read more »
Its most likely due to both SIBO and autonomic dysfunction
I’m curious if a symptom could be related to anxiety or the vagus nerve. I experience hot flashes, sweating, nausea (which I used to attribute to panic attacks) and I’ll usually have to run to the bathroom when this happens and have a BM or vomit, and a lot of time both. but now I’m wondering if it’s actually a symptom of something with the vagus nerve. It’s happened twice this month and before that once every few months. Those symptoms cause me to get scared and panicked obviously, but maybe they aren’t panic attacks like I’ve been thinking this… Read more »
It’s not the vagus nerve directly . An imbalance of intestinal bacteria is fully capable of triggering a panic attack and cause the vomiting and or diarrhea you describe.
Hi Dr N
i live in indonesia and in my country there’s no rifaximin available, is there a subtitute that i can used?
Not that seems to work as well.
Two questions : I’m confused about the mechanism of noradrenaline. If high noradrenaline levels contribute to anxiety, why are some antidepressants that are noradrenaline re-uptake inhibitors prescribed for anxiety? For example, amitriptylene. I have been taking 20mg of amitriptylene to address a sleep disorder (my body feels like it’s vibrating as I drift off/wake up from sleep) for a while now, but I’ve suffered increasing levels of anxiety during the day. I’m just about to buy your book, but I’m wondering if a low-amine diet is part of all this. My diet is definitely not low amine since I consume… Read more »
The high noradrenaline states entail massive systemic release of noradrenaline as compared the relative slight increases that occur between 2 cells communicating that happen with certain anti-depressants.
Hello Dr. Nemecheck, you mentioned “the third source of abnormal anxiety, the direct damage to cells within the portion of the brain that normally regulates anxiety, the amygdala. Some relief may be found in low doses of Acetyl L-Carnitine, an over-the-counter supplement that increases the production of reparative stem cells in the brain”
I am suffering terrible anxiety and panic attacks.
Would your adult protocol ca be used to reverse this source of anxiety?
Where can we purchase your adult protocol?
Kind Regards
Yes, my protocol was designed for adults.
Unfortunately the overwhelming response from the autism community is making it very difficult to finish the adult book.
But don’t worry, the dosing I recommend for adults with autism was specifically and originally designed for adults without autism.
Get the kids book and follow the adult doing recommendations.
I was interested in what you wrote about prebiotic fibre. I took some Bimuno (galacto oligosaccharide) a while ago, and all my anxiety symptoms went through the roof. I stopped taking it, and it returned to normal. I tried the same thing again month later, with the same results. Do you know why that might have been?
I also had a very strong nervous reaction to a pre-colonoscopy bowel prep, and wondered why that way too.
Could both these things indicate SIBO?
I find the beneficial effects of prebiotics in adults quite variable thats why I use rifaximin instead.
Hello Dr. Nemechek, I hope this message finds you. I am a 42 year old female, mother of one 14 year old son. In a nutshell, I have gone downhill since the birth of my son in 2004. Started with depression, but life was manageable until insomnia set in in November 2009. I had a severe panic attack in February 2010 which left me in a state of chronic insomnia, derealization, chroic fight/flight, panic attacks, brain fog and depression. I am paradoxical to all sleeping medications. When we finally found remeron which got me sleeping again, I got better and… Read more »
If can manage, finish the rifaximin and your symptoms will start to improve.
If you are too worried about the symptoms, contact the prescribing physician.
Hi Dr. Nemechek, I have been in and out of doctors offices and the er for the last 2 years Finally after numerous tests and visits I tested positive for SIBO. I also had a gastric emptying test with results consistent with autonomic dysfunction, as well as extremely low blood pressure and episodes of tachycardia and bradycardia. I started experiencing neurological symptoms first (numbness/tingling, dizziness, vertigo, migraine/partial seizure like episodes, headaches, fatigue. I had a TBI 23 years ago when I was 13 years old, followed by numerous concussions in early adulthood. I served 5 years in the military and… Read more »
The fish oil and olive oil can be started now but I generally tell patients to delay the use of rifaximin until after surgery because the procedure, anesthesia or associated antibiotic use might just cause a relapse anyway.
Hi Dr Nemechek, My 4 and 10 year old kiddos are on your protocol and doing great! I was recently diagnosed with central hypothyroidism in January and I’m taking levothyroxin for that. My question is pertaining to the adult protocol: I’ve been following the protocol and taking the fish oil, EVOO, inulin, and I’ve been eating nuts daily. I’m wondering if being on inulin is a good idea for me? I do not currently have access to rifaximin. I’m wondering if inulin is generally helpful in an adult or if it could end up stirring up more problems for me… Read more »
I generally don’t think the inulin causes problems in adults but it just didn’t seem to neutralize the inflammatory stress from bacterial overgrowth enough to allow for full autonomic recovery.
Thanks Dr. N.
Could I give my wife the Acetyl L-Carnitine at the same time, when starting the protocol?
Yes
Hi Dr. N,thanks for all the effort that you put in your work, i am wondering if the protocol could help my wife, she is 36, drinks a lot of coffee(+6 cups daily), “not so hard” things really affect her, like neighborhood noise, she is always over worried about everything, she can’t handle stress situations, i am not sure about what it causes those effects, i would really like to put her in test for the spectral analisys, but for us there is not really a possibility to travel to Arizona, we are from Ecuador (Sudamerica).
Yes it can help her very much.
If a child doesn’t have asd but does have delays/ sensory issues/ speech delay do they still require inulin as part of the protocol? Or can this increase anxiety?
Please read the protocol.
Thankyou Dr N I will start giving her Magnesium instead.
I watched your You Tube clip on adjusting the protocol to fit with extreme anxiety or aggression. She is a year into the protocol.
Do you believe adjusting or even omitting the inulin would help her anxiety/sensory issues?
Thankyou
Adjusting inulin will only help with anxiety or aggression issues. That being said, her tolerance of sensory issues will seeming improve if she is less anxious.
Thank you Dr N. We use 1/4 teaspoon of inulin daily and a high level of Nordic naturals omega 3 daily. We introduced movicol two weeks ago for severe constipation. The movicol helped her constipatipn, but, seems to have increased her anxiety and sensory issues. Thinking of trying magnesium. Is this pemitted for the protocol?
Magnesium doesn’t seem tp cause problems when used for constipation.
My child is 5. We have been on the protocol for 1 year. We are still seeing alot of anxiety. She has developed a habit plugging her ears when overwhelmed my her anxieties (particular animals, certain sounds and when she’s determined to get somewhere for example a park). Please could you offer any advice? Does she appear to still have sibo? Thankyou Dr N
There is either bacterial overgrowth or unresolved autonomic damage causing this.
If she is on inulin, you need to check his dosage and brand of fish oil and get rid of any additional supplements, probiotics, etc.
So inulin for adults is not sufficient? I feel like antibiotics got me here in the 1st place. Is inulin from Agave acceptable?
It’ll help the gut symptoms but it won’t be enough the help reverse underlying neurological damage.
My 13 year old non-verbal daughter with ASD, insomnia, irritability and SEVERE social anxiety has been on the protocol for about 6wks. We have seen great gains with her eye contact, nonverbal communication, she is more connected and less irritable. She still struggles to fall asleep night but her social anxiety seems to be getting worse. She has ALWAYS been anxious when out in the community even as a toddler but for the past few weeks she seems even more aware and it seems to be heightening her anxiety level. She has never tried to escape (run away) when in… Read more »
She sounds as if she has successfully entered the awakening phase.
Although I comment specifically about your child, the kids I treat often start having a reduction in their awakening symptoms around week 8 as long as the fish oil and EVOO dosages are adequate.
Dear Dr Nemechek, I have read your book and my 10 yr old daughter and I both went on your protocol a few days ago (me with the Rifaximin, she with inulin (twice a day 1/4 tsp). We both have high anxiety (mine on the verge of severe, the psychiatrist is looking into antidepressant options for me, which I do not want to get into) I have leaky gut, SIBO, hashimotos, high insulin levels etc. I had a ski accident – heavy blow to my head when I was 17 ( I am now 40) , a heart surgery also… Read more »
I recommend you read my protocol that was written for children with autism and developmental issues in mind.
It lays out all the issues you’ll both need to recover from generalized anxiety.
A copy can be found at https://autonomicrecovery.shop
Hi Dr. N, the panic attacks have gone and in place he is experiencing some auras (but much different than auras in the past). I am pretty certain his brain is changing. Although I can’t understand it, I hope it’s a good sign. This is a fantastic protocol! Thank you for responding to me!
It’s a good sign.