 Too many people are too hungry, and the result is a dangerous process called overnutrition.
Too many people are too hungry, and the result is a dangerous process called overnutrition.
Overnutrition doesn’t mean just too much nutrition, it means damage to the body by eating too much of a nutrient or substance. Examples disease cause by nutrients are blindness from vitamin A toxicity, heart failure from vitamin E toxicity, hypothalamus damage from vegetable oil and organ damage from excessive calorie intake (lipotoxicity).
Some toxicities such as vitamin A or vitamin E, are easy to avoid. Follow the recommended guideline when supplementing with vitamins and minerals. Others such as hypothalamus damage from vegetable oil are hard to avoid because these oils have been added to such a large array of foods we unknowingly are getting so much in our diets they damage our bodies.
These examples are somewhat controllable and avoidable. Don’t overdo the supplements, and clean up your food supply by limiting processed foods and preparing more of your meals with ingredients sourced from natural, healthy sources.
Unfortunately, limiting the consumption of calories can be a major challenge. It requires limiting your level of hunger which is much more difficult than it sounds.
Hunger is Not a Voluntary Sensation
Hunger is an innate signal designed to tell a primitive hunter-gatherer to find some nutrients to sustain their life. They had no sense of how much to eat or drink. Their brain told them what to do to stay alive. Feeling hungry is just as critical to survival as feeling thirsty, sleepy or needing to breath when underwater. All are primitive signals designed to keep animals alive.
Sometimes these survival signals can misfire and force us to behave in unusual ways, and even cause death. Excessive sleepiness is known as narcolepsy, and excessive thirst can sometimes result in seizure signaling mechanism.
The brain’s signaling can break as well. In patients with advanced HIV infection, their brains unfortunately tell them they are not hungry and don’t need to eat. This results in a weight loss disorder known as Wasting Syndrome.
More commonly, the brain will misfire and tell individuals to continue eating despite the fact they are just ate, and have plenty of available nutrients circulating within their blood streams. This state of excessive hunger is happening to a large portion of the population and is resulting in the disease process of overnutrition.
Overnutrition from eating too much food causes cellular damage to the body because the excess energy (calories) and other nutrients (saturated fats, linoleic acid, arachidonic acid) within the foods damage our body through the development of metabolic inflammation and insulin resistance.
Metabolic inflammation and insulin resistance are the process that ultimately trigger most cancers (breast, colon, skin, prostate), heart disease, stroke, Alzheimer’s and Parkinson’s disease, and many other less lethal problems.
Once your hunger is broken, it is difficult to withstand the urge to eat. Remember, this is a primitive signal designed to keep you alive, unfortunately its misfiring. Trying to eat less when your brain is telling you to do otherwise is like trying to breath only 10 times a minute instead of your usual 12 breaths per minute. It’s nearly impossible.
To try to restore hunger to a lower level it’s important to understand the variety of ways the hunger signaling mechanism can break.
Hedonistic Hunger
A first common mechanism and the one you can control the most is hedonistic hunger. Hedonism means the pursuit of pleasure or sensual self-indulgence. Hedonistic hunger occurs when you pass by the bakery counter at the local market and a donut or cookie catch your attention and you suddenly decide to buy a box although that’s not why you went to the market.
Consciously deciding to not bring a box of donuts, cookies or a half a gallon of ice cream home can limit damage brought on by hedonistic hunger. If it’s in the house, your brain remembers and will ultimately nudge you to eat them all whether it be in one day or over a few. Foods with high amounts of saturated fats and sugar tend to trigger this reaction.
Hedonistic hunger has an evolutionary basis in that if a hunter gatherer came across a patch of wild berries, honey in a bee hive or the high calorie content of animal fat, the brain would instruct them to eat as much of these foods as possible since they lived in a world where calories were not easy to come by.
My advice in this regard is to never bring these tempting foods into the house. If you want ice cream, go and buy 1 scoop at the ice cream counter, don’t bring a gallon home with you.
Hunger from Autonomic Damage
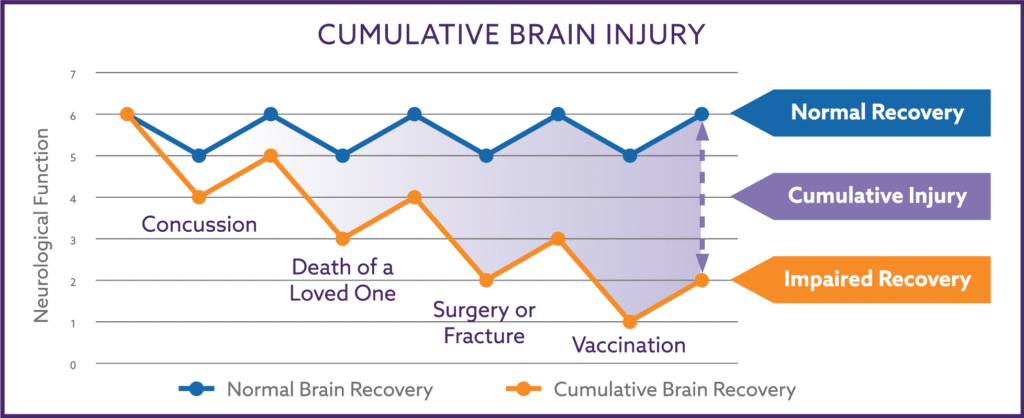
Another trigger of hunger is caused by low blood pressure and oxygen delivery to the brain as the result of damage to the autonomic nervous system. The brain senses there is not enough blood and oxygen being delivered, and views this as a threat to survival even though you only consciously experience the same level of low oxygen as fatigue, an occasional headache or lapses in concentration or memory.
Low brain blood pressure may be accompanied with a low blood pressure reading at the arm. But paradoxically, it can be associated with an normal or even high arm blood pressure reading in spite of having even low brain oxygen levels.
The brain believes its survival is at stake and will increase your sense of hunger especially for salty and sweet foods. These foods boost blood pressure to the brain and is joking referred to as the cravings for “pickles and ice cream” when women are pregnant. The low blood and oxygen levels also trigger what is misinterpreted as symptoms of “low blood sugar” in most individuals.
The low brain blood pressure will also increase a sense of thirst since even water if drunk fast enough will boost pressure and oxygen delivery. The effect of liquids is magnified if the liquid contains sugar, artificial sweeteners, or caffeine.
The hunger from low brain blood pressure is often also mistaken as “stress eating”. If the pressure in the brain drops enough, the body release noradrenaline in effort to boost blood flow to the brain. Noradrenalin also makes individuals feel very nervous or anxious.
These individuals then discover that eating foods high in sugar or saturated fats (often referred to as comfort foods) will alleviate the stress and make them feel better. These food are simply relieving the low blood pressure stress of the brain.
If you feel lightheaded occasionally, have any concentration or focusing issue (ADD, ADHD), generalized anxiety, recurrent headaches or chronic fatigue, or feel occasion allow blood sugar or weakness if you don’t eat on a regular schedule, your hunger is more than likely being inflated by low brain blood and oxygen levels. You might want to take our autonomic brain quiz to see if you might have autonomic nervous system damage.
Hypothalamus Damage Increases Hunger
The hypothalamus is an important, primitive area of the brain and amongst its many functions is its role in regulating hunger, sugar (glucose) metabolism, and where, how and if we can make body fat. an important aspect of hypothalamus function.
In animal studies, the hypothalamus can be damage in as few as 6 weeks when the animals ingest the same proportion of omega-6 fatty acids found in most vegetable oils and grain fed animals that are commonly consumed (think farm-raised fish, grain fed beef, chicken, turkey).
The omega-6 fatty damage the hypothalamus increases hunger, increase body fat deposition under abdominal muscles and in the buttocks, triggers insulin resistance causing pre-diabetes. Increased hunger from excessive omega-6 exposure is affecting a large portion of the general population.
As I written previously, supplementing with extra virgin olive as part of the Nemechek Protocol can go a long way towards reverse the hunger and fat distribution problems associated with hypothalamic damage.
Increased Hunger from an Imbalance of Gut Bacteria
A large proportion of the population are lacking a full range of bacterial species and some have in addition an imbalance of intestinal bacteria. The imbalance occurs primarily when bacteria that normally live within the colon are also living in abundance within the small intestine. This imbalance is often referred to as dysbiosis or bacterial overgrowth.
Transplantation of the intestinal bacteria in obese mice into skinny mice will cause the skinny mice to become obese. Likewise, transplantation of bacteria from thin, healthy men into obese diabetic men resulted in some improvement in their diabetes and obesity.
The abnormal distribution of bacteria can increase a person’s sense of hunger through a variety of mechanisms. Overgrowth can worsen low brain blood pressure from autonomic damage, alter the normal functioning of leptin and ghrelin, the normal hunger suppressing and initiating hormones.
Normalization of intestinal bacteria biodiversity and distribution with non-absorbable antibiotics, prebiotic fibers and fecal transplantation are all being studied as methods to reverse this form of increased hunger.
Hunger from Broken Fat Cells
Calories are a source of energy like electricity, and like electricity, have no weight in spite of the fact we put on weight when we eat too many calories. When we eat caloric energy, the excess energy available in the blood stream in the form of sugar or fatty acids are primarily stored in fats cells called adipose. A small amount is also stored in the liver and muscle.
Fat, the liver and muscle are the only places energy can be stored without ill effects. The energy from excess calories is similar in a fashion to the energy to run a nuclear power plant. The wrong amount in the wrong place is dangerous to all living organisms and can cause cellular damage and even death.
When stored in fat cells, the energy is accompanied by a certain amount of water. It is the additional water stored with the water and not the additional energy itself that causes an individual’s weight to increase when they eat more calories than they burn.
Moving energy from the blood stream into fat cells is an active process that requires certain receptors, enzymes and hormones to work correctly and in unison. There is a similar process for pulling the energy out of fat mass.
If things work correctly, the body will put energy into fat cells as well as allow the energy from fat cells to be released and converted into blood sugar between meals and when we sleep. Unfortunately, the process of releasing energy can also get broken when the hypothalamus is damaged.
In addition to excess omega-6 fatty acids, hypothalamic damage can occur with consumption of advanced glycation end products or AGEs. AGEs are unnatural molecules that develop when protein and sugars fused together due to heat and pressure.
AGEs are present in most of the cooked foods we eat with high concentrations being found in commercially prepared processed foods. Other than completely raw foods, AGEs will form in varying amounts when we cook our foods. In general, the higher the temperatures, the more AGEs are produced.
Excessive consumption of AGEs and omega-6 fatty acids disrupt the endocannabinoid system of the hypothalamus, leading to broken fat cells. Broken fat cells can function in a few ways. Some cells in under the abdominal muscles or around the hips and buttocks area will expand abnormally and can contribute to the overall inflammatory burden of the body.
In addition to inflate the hunger signal directly from the brain, damaged fat cells will increase hunger because they may not release the energy correctly between meals and result in a gradual hypoglycemic state.
In this scenario, the fats cells will take up energy but not let it go. The brain will try to compensate for the downward trend in blood sugar by inflating hunger even further.
Fat cells can also break in such a manner that they cannot grow larger no matter how much someone eats. This leads to the damaging effect of overnutrition for caloric excess.
Not All Excess Calories Go into Fat
Eating all you want without gaining weight may sound like a blessing but remember, the main safe place the nuclear energy of calories can be stored is within the fat.
If the fat cells don’t take up the excess energy within your blood stream correctly, this nuclear energy will flow into your brain and organs, and leads to a state described by metabolic experts as overnutrition.
Overnutrition is a critical component in the development of many common illnesses such as fatty liver disease, heart failure from cardiomyopathy, diabetes mellitus type 2, metastatic cancer, autonomic nervous system dysfunction as well as Alzheimer’s or Parkinson’s disease.
People experiencing overnutrition from excessive caloric exposure have 4 major patterns.
The first is a rare pattern of an individual whose hunger is broken but their fat cells seem to suck in all available energy but don’t release the energy as readily when it’s required. This pattern is rare but leads to excessive hunger and weight gain. Despite gaining enormous amounts of weight, they do not develop any metabolic effects from overnutrition (insulin resistance and metabolic inflammation) since they store all the excess energy safely in their fat cells.
Their labs tests and blood pressure will remain generally normal despite their super morbid obesity but they often end up developing heart and orthopedic problems from the mechanical effects of their sheer size.
These people are sometimes referred to as obese but metabolically healthy. Most individual with broken fat start down the path of being able to store all excessive energy but their fat cells eventually falter, and are unable to store all the excess energy. This second pattern is when the damaging effects of overnutrition begin.
The second pattern still gains weight from excessive caloric energy but a portion of the energy is unable to be stored correctly and flows into the brain and other organs. The second pattern may progress along this path for a decade or 2 without anything serious occurring medically.
They will develop some minor abnormalities in their blood work such as elevated triglycerides, blood sugar or mild elevations of their liver enzymes, and will experience some medical conditions from abnormal hormonal fluctuations such as hypogonadism, polycystic ovarian syndrome, infertility or gynecomastia.
Eventually something serious will occur in 2-3 decades or their progression into overnutrition may accelerate into the third pattern. In this pattern, fat cells completely lose their ability to store energy and all excess energy begins flowing into the brain and organs.
This third pattern is occurring when the individual realizes their weight doesn’t seem to increase no matter what they eat. Patients realize that they reach a certain plateau of body weight, and then from that point forward they don’t seem to gain a pound no matter how much they eat. They are sensing the inability to grow their fat mass any longer.
This is very dangerous because now all the excess nuclear energy they consume is now flowing into their brain and organs instead of being safely stored in fat. Overnutrition is kicked into overdrive and progression to disease, disability and death accelerates.
Although most individuals experience the second pattern to some degree, most will not slide into the third more dangerous pattern.
The third pattern often occurs around 35-55 years of age but the complete failure of energy uptake by fat cells can also occur much earlier in life and represents the fourth pattern. Individuals with this fourth pattern are often mislabeled as having a “high metabolism”.
The typical individual with the fourth pattern of fat cell failure is the young individual often in their 20’s who is constantly hungry, eats more than anyone at the table yet doesn’t gaining any weight. These patients may develop sleep apnea, infertility or aggressive metastatic cancer at an early age despite appearing thin and healthy.
How to Reduce Hunger and Reduce Body Fat
By now you realize that trying to lose weight and remain healthy are nearly impossible goals if your hunger is abnormally inflated and your fat cells can’t protect you from excessive caloric energy.
The Nemechek Protocol is specifically designed to address the damaged metabolic mechanisms that result in inflated hunger and the inability of fat cells to protect us from excess caloric energy.
Over time, patients utilizing the Nemechek Protocol will realize their snacking and episodes of “low blood sugar” eventually stop. As their sense of hunger in reduced their energy, cognition and other physical ailments begin to fade away as well.
Over time they can begin reducing the carbohydrates in their diet and notice they can skip a meal such as breakfast without feeling weak or shaky. And eventually they incorporate intermittent fasting that triggers the body to release abnormal and excess stores of body fat.
This post is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be patient education, does not create any patient-physician relationship.
© 2017. Dr. Patrick M. Nemechek and Jean R. Nemechek. All Rights Reserved. Patent Pending.
Thank you Dr N! He is 8 but weights nearly 100lbs now. I agree on paleo not necessarily being more healthy but with the weight gain we are trying to substitute white flour with lower carb options…it’s desperate times. Doctors say it’s just him and a slower metabolism but I refuse to accept that. If you think SIBO is the cause it sounds like we need to come for a visit with you unless it is the supplement doses that just need to be adjusted. I should add he also has asthma. Thank you!!
We have been on the protocol with my son since July for constant hunger, thirst, fatigue, abnormal weight gain, immune deficiency (low IgA and WBC’s) and I have noticed no progress, in fact his weight is getting to be more and more of a problem despite healthy diet changes(implementing Paleo and using EVOO as cooking fat…gluten, dairy, and grain free), he is very active in sports etc… is it a possibility we are barking up the wrong tree with SIBO or do we come see you to figure it out? He is on 5ml’s of Omega 3’s, 1tsp inulin, and… Read more »
You doses are dependent on your son’s age and occasionally I need to use rifaximin in children when inulin does not help.
I don’t necessarily agree that paleo diets are somehow healthier than other approaches.
I just found your page. I’m engrossed. I am pretty certain I’m dealing with SIBO but had no idea about ANS. In fact I worked with a nutritionist in the fall and did an intense elimination diet along with some herbals to kill the bad bacteria. While my symptoms reduced, I still lost no weight, despite cutting sugar, dairy, all grains but oats and Quinoa and FODMAPs, and hunger remained a factor. My low thyroid is being treated, so that’s been examined. I believe, that having a traumatic natural birth in 2010 and then a stillbirth in 2013 both complicated… Read more »
This is fascinating to me…I belong to a group of parents of children with ADHD, and so many of our kids have food obsessions, sneak food in the middle of the night, and many are overweight. My own daughter (ADHD-combined type) was also constantly hungry from her first days of life, and I actually had to stop feeding on demand or she would eat till she made herself sick. We just started the protocol a couple of weeks ago, and now I’m wondering whether it will help with her hunger as well as her ADHD. It’s so interesting to see… Read more »
Both abnormal blends of intestinal bacteria, hypothalamic damage from omega-6 oils and AGEs and autonomic dysfunction all can cause increased hunger, cravings.
I’m uncertain about autonomic dysfunction or omega-6 toxicity right at birth but the bacterial issues can be there right from the start.
Thank you so much! Does the 500/600 calories during intermittent fasting include the fish/olive oils?
I don’t count them because the omega- fatty acids in these oils are not readily available as an energy substrate. They are first incorporated into cell membranes and more than likely are not available as a calorie for energy for 24-48 hours.
First I want to thank you for sharing so much of your valuable information. I am so grateful for your work and generosity with your knowledge! My ADD and SPD daughter and I have been on your protocol for over 4 months and both of us have seen some great gains along with a lot of patience . My gains include better digestion(could not fully digest raw veg, smoothies), severe coccyx pain after birth of my fifth child 2 1/2 years ago has DISAPPEARED and I’m feeling fuller longer! Along with these positives I seem to be gaining weight since… Read more »
I’m delighted you and your daughter are doing so well. It’s amazing what a little reduction in inflammation can do.
A little weight gain at the beginning occurs sometimes and I am uncertain if this is due to better absorption of nutrients, a normalization of adipose function or normalization of hypothalamic function or all three.
As autonomic recovery continues, I have patients reduce carbs to 100 grams per day max, then incorporate time restricted feeding (skip breakfast and eat calories between 11 and 8) and the add intermittent fasting twice weekly (only 500/600 cal for 24 hours for women/men).
Dear Dr. N,
My 10 year old seems to be in the fourth pattern his whole life. Only now, after starting your protocol, is he able to fast for reasonable amounts of time without going into total meltdown. Do you believe this is possible, to just be born with this fourth pattern you describe?
Yes, I do. I think any of these patterns can be apparent early in life.