The last few decades have seen an alarming increase in acquired neurological disorders among children. Children increasingly develop conditions such as autism, developmental delay, sensory problems, emotional disorders, attention disorders (ADD/ADHD), post-concussion syndrome, tics, Tourette’s syndrome, PANS, and PANDAS. Here’s what you need to know about PANS, PANDAS, and Autism.
Acquired neurological conditions develop after birth and are viewed differently from congenital disorders that may have a genetic component or have occurred before birth. Consequently, researchers are grappling to understand each of these conditions, but unfortunately, they often focus on individual disorders and not the bigger picture. There is little to no research on understanding why such a large variety of neurological conditions increasingly affect children over the same time frame.
Commonly Acquired Neurological Conditions
- Tics
- Autism
- PANS/PANDAS
- Attention Disorders
- Emotional Disorders
- Tourette’s Syndrome
- Developmental Disorders
- Post-Concussion Syndrome
When assessing an individual who develops a variety of symptoms within a relatively narrow timeframe, a physician is trained not to view each problem or symptom separately but to look for a single cause that might be responsible for all their symptoms. Applying the same logic to the increased acquired neurological issues in children, I think small intestine bacterial overgrowth (SIBO) could be the single common factor contributing to these conditions.
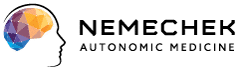
SIBO is a condition in which bacteria that typically live within the colon are found in high concentrations within the small intestine. The small intestine typically has relatively few bacteria, but SIBO results in bacterial counts ranging from 1,000 – 100,000 times the amount normally found. Besides contributing to some digestive issues such as diarrhea, reflux, and food intolerance, SIBO results in the leakage of molecules of nutrients and bacteria into tissue layers surrounding the small intestine.
The small intestine wall disruption is called a bacterial translocation (i.e., leaky gut) since only bacteria cause this. Yeast (i.e., fungi, Candida), viruses, and protozoa (i.e., parasites) may grow in excess within the small intestine, but there is no evidence they contribute to the leaky gut problem.
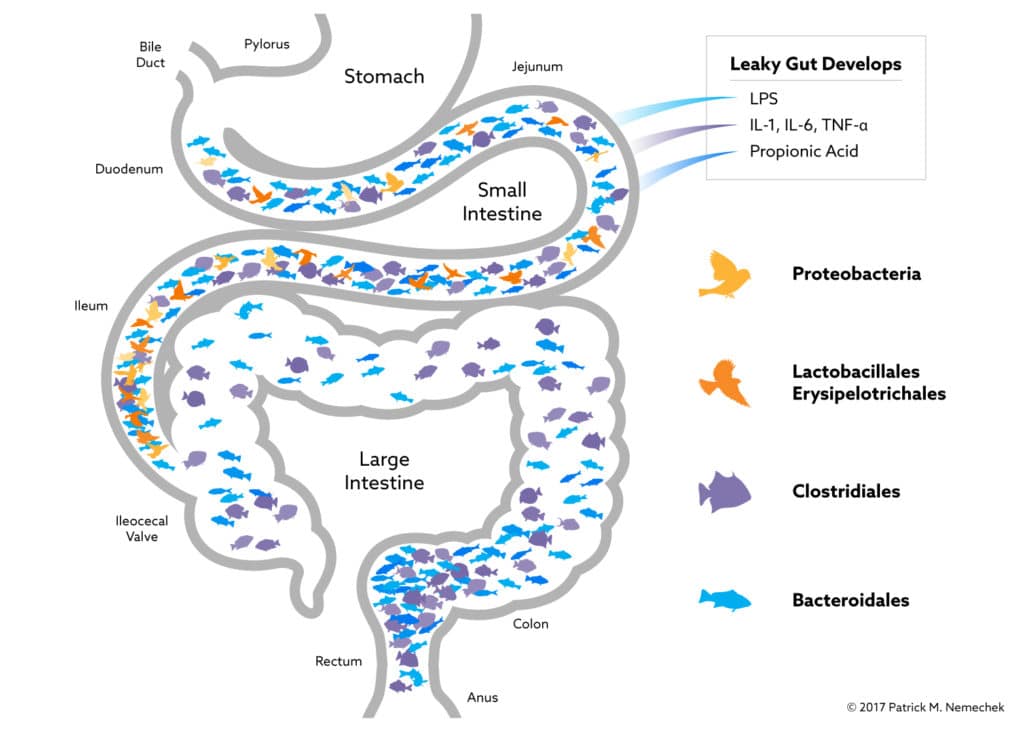
I can explain SIBO’s ability to trigger various neurological disorders in children through two factors, the age when bacterial overgrowth first occurs and whether or not the overgrowing bacteria can produce a behavior-altering substance such as propionic acid.
For normal neurological development in a child to occur, the brain’s neuron mass is pruned from approximately 100 billion neurons down to 50 billion by the time the child is five years old. Inflammation from SIBO can prevent the pruning from occurring correctly. If SIBO occurs before five years of age, the child will have some developmental or sensory issues. If it occurs after five years of age, no developmental problems arise because the pruning is already complete.
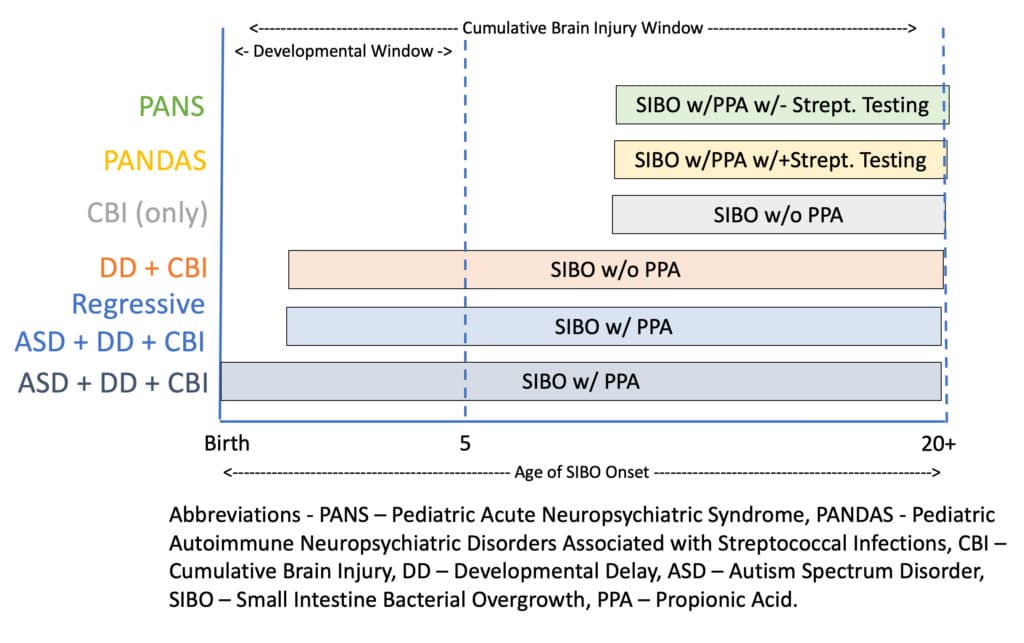
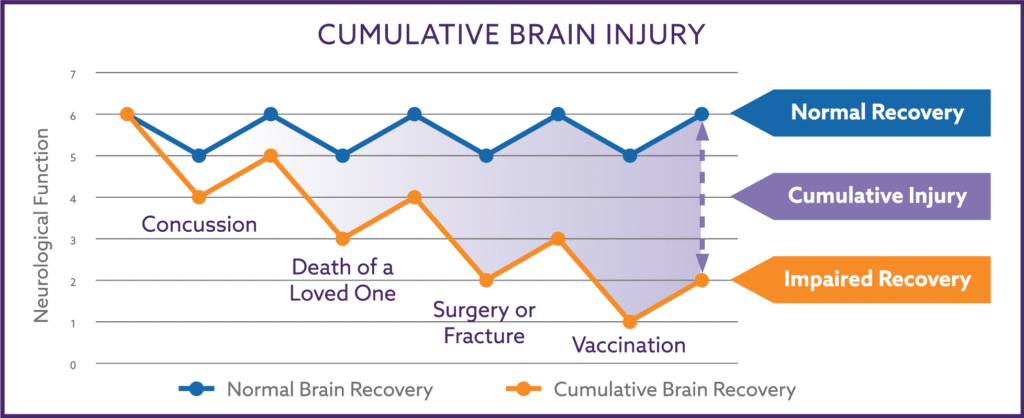
Inflammation from SIBO can prevent the brain from repairing itself after an injury, resulting in residual neurological damage after each injury. Over time, the unresolved injury from repeated traumas will build on top of each other, resulting in a cumulative brain injury or CBI phenomenon.
Symptoms of Cumulative Brain Injury (CBI) in Children
- Bloating
- Insomnia
- Anxiety/OCD
- Constipation
- Hyperactivity
- Heartburn/Reflux
- Chronic Depression
- Focus/Attention Disorders
- Aggression/Temper Tantrums
- Increased levels of Thirst or Hunger
Unlike the pruning process, cumulative brain injuries can occur throughout life. Therefore, whether or not the inflammation from SIBO occurs before or after age five, CBI increases with each additional injury.
SIBO Before 5 Years of Age
If SIBO occurs after age 5, a child can only develop cumulative brain injury. If SIBO occurs before age 5, the child will always experience CBI and developmental delay. Depending on the intensity of the inflammatory strain caused by SIBO, the developmental issue can be mild or severe.
Propionic acid (PPA) is found in high concentration in the tissues of children with advanced autism and has a sedating and, at times, almost hallucinatory effect on the children.
The production of PPA is dependent on the specific colonic bacteria that is overgrown within the small intestine. Since not all colonic bacteria produce propionic acid, the excess production of PPA depends on whether or not the overgrowing species is capable of excreting it. If the overgrowing bacteria produce PPA, the child will have decreased awareness and poor eye contact and may engage in strange behaviors such as staring transfixed at spinning objects.
Effects of Propionic Acid on Children
- Poor Eye Contact
- Preference to Be Alone
- Decreased Awareness
- Repetitive Behaviors
- Obsession with Spinning Objects
A child younger than five years old with SIBO with a PPA-producing species of bacteria will have developmental issues, cumulative brain injury symptoms, and behaviors uniquely associated with autism. If younger than the age of five, when SIBO occurs with a bacteria that does not produce PPA, then the child will not have these unique autistic behaviors and will only be diagnosed with developmental delay and cumulative brain injury.
SIBO After 5 Years of Age
After age five, SIBO without PPA production will result in cumulative brain injury symptoms and no developmental issues. If the child is older than five years old, SIBO occurs with PPA-producing bacteria, they will manifest in conditions commonly referred to as PANS (pediatric acute-onset neuropsychiatric syndrome) or PANDAS (pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections).
The symptoms commonly associated with PANS and PANDAS consist of high anxiety levels, often resulting in obsessive-compulsive behaviors (i.e., OCD) and other neurological and psychiatric symptoms. The main difference is that PANS have a rapid onset, often within 24-48 hours. In contrast, PANDAS does not develop rapidly and is associated with colonizing streptococcal bacteria in the pharynx (i.e., a positive strep throat swab). PANS and PANDAS can mysteriously disappear as quickly as they appear and reappear months or years later.
I believe both PANS and PANDAS are simply the occurrence of SIBO with PPA-producing bacteria and are not separate medical conditions. In animal studies, SIBO increases anxiety-like behavior, and I have witnessed this same effect in my private practice. A subset of my adult patients will also experience high anxiety levels after SIBO develops. The anxiety can rapidly resolve after treatment of SIBO with rifaximin (Xifaxan®). Many of these adults had their anxiety initially escalate very rapidly after an infection, a course of antibiotics, surgery, or a brain injury, all of which are well-known triggers of SIBO.
The confusion with PANS and PANDAS is that the spontaneous resolution of these conditions after a course of antibiotics lies in commonly used antibiotics, such as amoxicillin or trimethoprim/sulfamethoxazole have a 20-30% chance of reversing SIBO. Thus, their use can sometimes lead to rapid symptom improvement and even complete remission.
Suppose a physician managing a child with PANS or PANDAS is not tracking every course of antibiotics that other physicians might have prescribed the same patient for a routine middle ear or dental infection. The common antibiotics used in these instances can reverse SIBO and trigger an improvement in the patient’s PANS or PANDA symptoms. The physician commonly misses the real reason for the child’s improving symptoms and considers their progress as “spontaneous” or a consequence of some other treatment (vitamins, homeopathy, heavy metal therapy, etc.).
Positive Strep Tests Don’t Always Mean What You Think
Also, the diagnosis of PANDAS requires the presence of a positive streptococcal throat test or culture in children. Approximately 10% of all children within the U.S. are carriers of harmless strains of streptococcus, test positive with rapid strep tests or throat cultures, and do not have any symptoms. Infectious disease specialists advise against treating these children with antibiotics because they are often incapable of clearing the streptococcus and do not benefit their health.
Because of the high carrier rate, 10% of any group of children with any common disorder will carry streptococcus. Because of this, streptococcus can mistakenly be linked to almost any disease process using this logic. What further leads physicians down this path of mistaken therapy is that prolonged courses of antibiotics they treat children with can partially suppress SIBO and reduce PPA production, resulting in some improvement in the child’s symptoms.
The faulty logic of “giving antibiotics for streptococcus bacteria leads to improvement; therefore, the problem is caused by streptococcus” is understandable but incorrect. Treating the same child with rifaximin has a better and longer-lasting positive response. And since rifaximin does not enter the bloodstream, the positive impact from rifaximin cannot be because it cleared the throat’s streptococcus infection.
Autoimmune Versus Autoinflammatory
While I agree that children diagnosed with PANS or PANDAS have excess inflammation within their brains, I disagree that this is an autoimmune process; the children suffer from an autoinflammatory process. Inflammation from an autoimmune process targets specific types of tissue in the body. For example, rheumatoid arthritis is an autoimmune disorder in which inflammation is primarily located in just a few particular joints of the hands. Think of autoimmunity as a sharpshooter who can hit the center of a bullseye when shooting a bullet without damaging other bodily systems.
Autoinflammation is the release of inflammatory chemicals into the bloodstream, and these chemicals have wide-ranging adverse effects on the tissue of the body. In the case of the hands, almost all the joints of the hand would hurt, and not just a specific few joints as seen in rheumatoid arthritis. Instead of a sharpshooter, think of autoinflammation as a shotgun that cannot just hit the target’s center but instead scatter its effect across a much larger area.
When SIBO is present, the leakage through the small intestine walls can activate up to 80% of all white blood cells. These cells, in turn, release inflammatory chemicals called cytokines into the bloodstream and potentially harm any cell from head to toe.
Besides, the reversal of SIBO with rifaximin causes a rapid reduction in autoinflammation and PPA levels and results in the sudden improvement of my patients mistakenly diagnosed with PANS and PANDAS. Historically, treating most autoimmune disorders results in a slow reversal of a patient’s symptoms.
The Effectiveness of Nemechek Protocol®
I have assisted in caring for almost 700 children with autism, developmental delay, sensory issues, and cumulative brain injury, many of which had been previously diagnosed and treated for PANS or PANDAS. The Nemechek Protocol® is focused on reducing inflammation, most notably through the reversal of SIBO using either the prebiotic fiber inulin or the non-absorbable antibiotic rifaximin.
My protocol allows more than 90% of the children under my care to maintain a rate of neurological recovery that parents, teachers, and therapists find unequaled. My protocol’s true power and success lie within the human body’s natural ability to neurologically recover if the body is maintained in a healthy, non-inflammatory state.
This post is provided as an information resource and is not to be used or relied on for diagnostic or treatment purposes. This information is not intended to be patient education and does not create any patient-physician relationship.