 Some women suffer for decades after menopause. But what if we approach it like a traumatic brain injury or a concussion?
Some women suffer for decades after menopause. But what if we approach it like a traumatic brain injury or a concussion?
What if relief lies in repairing the brains and nervous systems of these women just like repairing the brains and nervous systems of male pro-athletes?
There are new treatments for postmenopausal women, turning off hot flashes and night sweats, as well as reversing recurrent urinary infections and dryness problems.
It is now possible to correct neurological issues by promoting key brain repair months or even decades after the onset of menopause.
Too many women are handed hormones and told to just live with it. That is unacceptable inattention to their medical issues without getting to the root of their problems.
It also leaves me with the nagging question if our great grandmothers lived without hormone replacements, why are modern women told they need them?
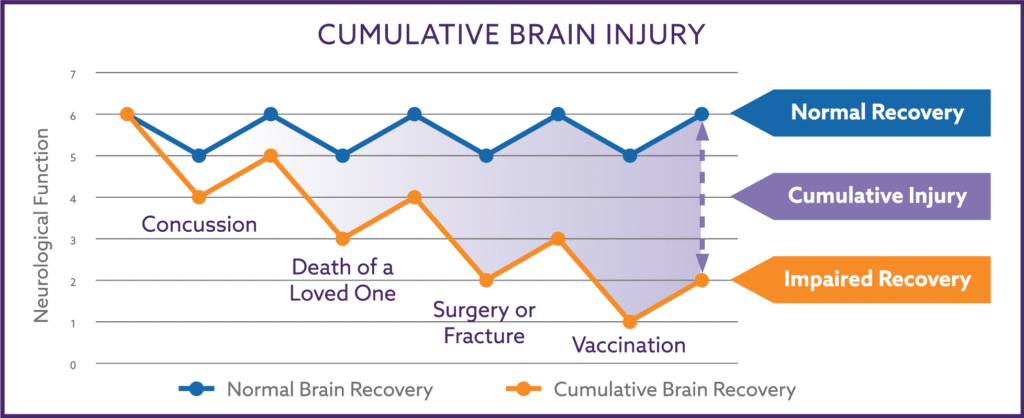
The answers may be found in the fact that some women quickly recover from menopause symptoms, while others suffer forever – just like unresolved brain concussion damage.
We must first redefine menopause. Menopause is more than the drop of hormones when childbearing years end. Menopause symptoms arise from a damaged Autonomic Nervous System after repeated traumas, nutritional stress, and metabolic inflammation.
Scientific studies are beginning to connect these dots, and I have been developing Autonomic recovery techniques for years.
In many respects, menopause is permanent PMS (Premenstrual Syndrome).
In my experience, the symptoms of PMS and menopause are due to magnifications of prior physical or emotional concussion damage because of changes in levels of progesterone and estrogen.
These are not just simply hormonal imbalance problems; these are actually reversible mechanical brain and Autonomic Nervous System problems.
In PMS, the decline of progesterone and estrogen that occurs before the onset of menstruation will worsen the symptoms from low brain oxygen levels from a prior concussion.
The only main difference is PMS symptoms only last for a few days but repeat every month, while the symptoms of menopause may unfortunately goes on forever unless until their Autonomics recover.
Menopausal women also experience the decline in progesterone and estrogen as seen in PMS except that it is permanent, and is due to ovarian failure.
And similar to the younger PMS women, their worst post-menopausal issues (weight gain, anxiety, fatigue, and persistent headaches) are tied to the sympathetic branch of their Autonomics.
So what does Autonomic Nervous System recovery do for postmenopausal women that mere hormone replacement does not?
The Autonomic Nervous System is the portion of the nervous system involved with the coordination and regulation of all organ function, metabolism, hormone regulation, and inflammation.
When the Autonomics fail to work properly the bodies’ response to disease and stress are impaired. Once the Autonomics are injured, the brain develops problems that include regulating blood pressure and brain oxygen delivery, moving the digestive tract, maintaining normal heart rhythms, temperature regulation, and proper organ and immune function.
The Sympathetic branch of the Autonomics controls our “fight or flight” nervous system response, so the common complaints of sympathetic dysfunction include headaches, heartburn, anxiety, insomnia, tingling or numbness of the arms/hand/feet/face, and chronic hunger, pain, and fatigue.
In PMS, the drop in hormones right before a woman’s period magnifies their underlying sympathetic Autonomic dysfunction. And as the hormone levels begin to increase again as they cycle, oxygen delivery to the brain improves somewhat and their symptoms lessens.
This occurs over and over with each menstrual cycle until the cycles stop with menopause. At that point the oxygen delivery crisis becomes a state of permanent PMS.
The PMS women in my practice all show damage to the sympathetic branch of the Autonomics when I test their nervous system using spectral analysis.
Sympathetic damage is the most common form of Autonomic brain injury and sympathetic damage is measurable for decades after an emotional or physical concussion.
Sympathetic dysfunction, without prior surgery, is why some women develop varicose veins. The sympathetic branch is responsible for the normal constrictive tone in the arteries and veins.
A lack of constrictive tone, after sustained sympathetic dysfunction, leads to venous dilation. In other words, the valves get damaged and the blood is not pumped correctly out of their legs. This can greatly improve as sympathetic damage normalizes.
Sympathetic damage is also why some women experience increased intra-abdominal fat. Cortisol, a stress hormone, is released by the body to push blood to the brain which gets harder to do as the sympathetic dysfunction worsens over time.
As the damaged sympathetic system works harder to try and get blood to the brain, more cortisol is released. A side effect of cortisol is an increase in fat under the abdominal wall muscles. Excessive body fat and cortisol levels will also improve with Autonomic recovery treatment.
When the sympathetic branch fails to operate correctly, the important sympathovagal balance between the two branches is disrupted and additional problems or symptoms may then develop from the parasympathetic branch not working correctly.
Parasympathetic failure causes hot flashes and night sweats, intolerance to light because of dilated pupils, inadequate inflammation control leading to chronic pain and autoimmune disorders, intestinal bloating and constipation, and urinary urgency and incontinence because of poor bladder function.
Supplementing with hormones in the form of birth control pills, post-menopausal replacement therapy will improve the symptoms from low oxygen delivery but those pills come with the risk of increased blood clotting, heart disease, and possibly breast and uterine cancer.
The pills also do not heal or reverse the underlying sympathetic or parasympathetic Autonomic damage.
Autonomic recovery is attainable with an individualized plan including traditional pharmaceuticals when necessary, vagal nerve stimulation/electronic acupressure, the elimination of bacterial intestinal infections, cleaner and more nutritious foods, and a very limited amount of supplements that mimic our great grandmother’s natural omega 3 food sources.
Relapse of Autonomic damage is common if compliance with the nutritional changes is not continued. Because of this, yearly retesting is advisable to monitor sustained sympathovagal balance within the Autonomic system.
Sympathovagal balance between the sympathetic and parasympathetic branch is not just important for concussion recovery and the elimination of menopausal symptoms. Sympathovagal balance is necessary for long, healthy life.
My goal is not just to help these women feel better today, but to restore Autonomic functioning because it is critical to their life expectancy. Improved Autonomic function improves their heart rate variability (HRV), a measure of overall health.
People with elevated HRV have an increased risk of developing atrial fibrillation or heart flutter. People with low HRV have an increased risk of widespread organ and metabolic dysfunction.
Low HRV is an indicator of increased risk of mortality from all causes, in both men and women.
As a scientist physician, I use every tool and technological advancement available to coax the body to naturally repair the sympathetic Autonomic damage resulting in improved oxygen delivery, the reversal of the associated PMS symptoms, and eliminating the need of supplemental hormones.
Menopause is permanent PMS, but with consistent effort Autonomic recovery will result and The Change will not be how things remain until The End.
I am an internal medicine physician with expertise in Autonomic Nervous System testing and Autonomic recovery located in the Phoenix, Arizona area. For more information you may contact my office at 623-208-4226 or visit my website www.DrBuckeye.com.
© Copyright 2015. Dr. Patrick M. and Jean R. Nemechek. All rights reserved.
Dear Dr. Nemechek, I have been on The Protocol for seven months now, to the letter, including three rounds of Rifaximin. I’ve seen my anxiety improve tremendously and am back at work after wondering if I could ever handle the stress again. I also feel relief from PMDD for the first time in decades. I am deeply grateful for these changes. Other benefits seem to elude me still. Between having very low cortisol and SIBO, and being hypothyroid and estrogen dominant, my energy and stamina have declined, I’ve lost my libido, muscle mass, and I remain quite constipated. I am… Read more »
Can’t tell anything else to do but call and get placed on the cancellation list.
If you’re flexible, appointments sooner than July become available all the time.
Hi Dr. N, I’m 41 and have been on BCP for 20 years (minus the ~2 years when I was trying to conceive and pregnant). Off the pill, I am highly prone to ovarian cysts, with one incident of a ruptured cyst requiring emergency surgery. However, I’d like to be free from hormones at this point, plus I am experiencing benefits from having started your protocol a few months ago. Do you have a recommendation for a way to avoid cysts without taking hormones? Could the protocol help? My doctor just started me on the minipill as an alternative to… Read more »
I don’t have any experience with the effect of the protocol on the recurrence of painful ovarian cysts.
That being said, the autonomic nervous system controls inflammation as well as all hormonal regulation and improvement in autonomic function may very well improve the pain from ovarian cysts.
Hello, I am writing for my 49 year old wife on her behalf. She is Pre Menopausal and has been for the past 5-6 years. As the years progress, her symptoms seem to worsen. As of now, she is scheduled to get a historectomy. The reason is because she was diagnosed with (Endimiosis which is the lining of her uterus is growing). This is causing her heavy long periods with pain. This has caused her to be a nemic. Doctor is giving her an option to remove ovaries but for sure will be removing cervix, uterus and fallopian tubes. The… Read more »
Steve,
You wife’s situation is very complicated as is the decision about removing the ovaries. As you probably realized in reading this article, much of the fatigue, brain fog, moodiness, increased hunger and weight, anxiety is often from underlying autonomic dysfunction that is worsened with lower levels of progesterone.
All I can suggest is follow your surgeons advice about resolving the endometriosis and the pain and anemia that accompanies that and then look for ways to restore your wife’s underlying autonomic dysfunction to help with any remaining symptoms.
I am 35 yrs old and having perimenopausal symptoms from age 28. The reason being, one of my ovaries was removed due to a huge cyst at age 20. At age 29, I conceived naturally and gave birth to a baby boy. My Perimenopausal symptoms started with digestion problem, gas, and bloating which gradually moved to constant fatigue, depression, skin itching, sleeplessness, brain fog difficulty in breathing, frequent cycles, scanty bleeding, headaches, irritability, difficulty in socializing etc. Earlier I did not realize these as premenopausal symptoms and always wondered that i might have serious digestive problem or just stress. I… Read more »
As I discuss, many of the chronic symptoms associated with menopause are related to autonomic dysfunction
I am 52 and have been in menopause since I was 45. I have all these symptoms with a few added problems. Super high testosterone levels (I have always had) . I also have 2 brain lessons that are stable, 1 is in my third ventricle the other is in occipital lobe. I am super tired all the time depression is horrible, I don’t even like going outside anymore. I am scheduled for a complete hysterectomy because my uterus has grown 4 times the normal size. But none of the Doctor’s Can figure out what is going on because all… Read more »
As your read in my article, the main symptoms attributable to PMS and menopause arise out of damage to the autonomic nervous system that did not get repaired. Sympathetic damage is a common source of fatigue, headaches, poor concentration, poor memory, increased hunger or snacking and generalized anxiety. Chronic depression on the other hand is chronic, unrepaired damage to the hippocampus, the region of the brain that controls emotions. The autonomic nervous system controls almost all hormones. Sounds like you need to make a trip to Arizona so we can get your autonomics to repair and get you feeling better… Read more »
I am 64 and still suffering from menopausal sweats. What specific steps can I take in diet and supplements to help alleviate? Thanks.
Try taking a prebiotic fiber. Many women with post menopausal sweats simply have SIBO as a cause. The other cause seems to be related to abnormal parasympathetic function, and this is much more complicated to repair.
Dr. N