 Headaches come in many forms
Headaches come in many forms
It is important to find out where are someone’s headaches located, and what time of the day do they start?
Some headaches affect the front or the back of the skull, some start with tight neck muscles and pain that travels, others start when someone first wake ups while they are still lying in bed, and others do not start until after someone has gotten up in the morning or later in the afternoon.
I try to classify a patient’s headaches into 4 different categories; low blood pressure headaches, sinus headaches, inflammatory headaches, and unknown. My approach helps organize headaches according to the underlying cause because once you understand the process, finding methods to prevent headaches becomes easier.
Low Blood Pressure Headaches
The first type are low blood pressure headaches are these are very common in many people. These headaches start at the back of the head and are often accompanied by neck tightness or pain.
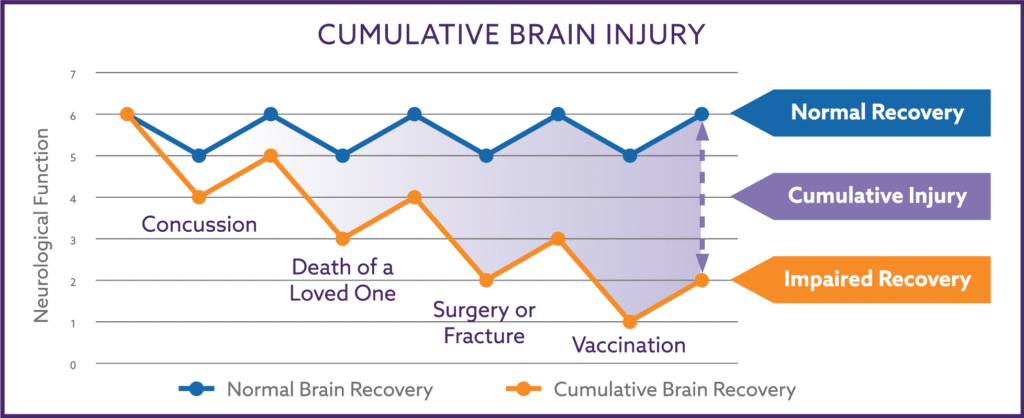
Many people are suffering from chronic yet reversible injury to their Autonomic Nervous System, and they have relatively low blood pressure in their shoulders and head. Strangely, a person with low blood pressure in the head and neck may have low, normal, or high blood pressure readings when their blood pressure is measured in their arm at a doctor’s office.
The low blood pressure into the muscles of the neck, scalp, and jaw, results in tightness and pain because of a lack of oxygen. “Coat hanger pain” is the specific term coined for the neck and shoulder tightness, and it means if someone held a coat hanger up next to their shoulders, neck, and the back of their head this is the area where many people experience discomfort and pain from low blood pressure headaches.
The pain can radiate forward from the neck through the other muscles of the scalp. In some cases, the pain originates from the muscles of the jaw with pain being felt on both sides of the head in the temple region or the jaw. This is often misdiagnosed as TMJ pain (temporal-mandibular joint).
Low blood pressure headaches occur only after a person has sitting or standing in the upright position for a while. People do not have these when lying flat in bed in the morning but these headaches may start after getting up out of bed. And as the day wears on, the blood pressure into the neck and scalp muscles slowly worsens so these types of headaches often occur in the afternoon.
Children frequently get these low blood pressure headaches during the last few periods of class at school after they have been sitting still at their desks. Other situations that can trigger these types of headaches in children or adults may be during long car rides, airplane rides, or after getting a little overheated.
Low blood pressure headaches may become so severe that they are referred to as “migraine” headaches. Laying down helps to lessen these headaches because laying down eliminates the challenge of gravity on our body, which makes it easier to pump blood into the scalp and neck muscles.
Other clues that someone may have low blood pressure headaches is occasionally feeling lightheaded, fidgety, experience troubles with focusing and concentration, have episodes of “low blood sugar”, or have generalized anxiety. These are all other symptoms of low brain blood pressure that may or may not happen at the same time as the headache.
In my internal medicine practice, I test and treat the Autonomic Nervous System. The cause of the low blood pressure headaches that I see in my patients are caused by autonomic dysfunction and not by narrowed blood vessels. But there are two other medical conditions that people should discuss with their physician, Angina from heart disease and claudication pain from peripheral vascular disease, that have similar sources of muscle pain due to lack of oxygen.
Sinus Headaches
The second type are sinus headaches. Sinus headaches happen when the mucous membrane lining the nasal passage and sinuses swells enough to block the opening to the sinuses. Once the opening to the sinus is blocked, the mucous membranes absorb the gases within the sinus leading to a vacuum that triggers pain.
Sinus headaches most often occur in the front half of the face, worsen with changes in weather because of shifts in barometric pressure, are more frequent with worsening allergy symptoms, can occur when first waking in the morning, and often improve or resolve a short while after getting out of bed.
Some people do not make the connection between their sinuses and their headaches because they think if their headaches were related to their sinuses that they would have other sinus symptoms. But one does not need to have a lot of sinus drainage or obvious nasal congestion to experience sinus headaches. Short term or over the counter nasal sprays may open the sinus enough to relieve the pain and stop those types of headaches.
Inflammatory Headaches
The third type of headaches are inflammatory headaches. Inflammatory headaches often have a very diffuse pattern of pain that a patient describes as “hurting all over”. Unlike low blood pressure or sinus headaches which respectively start at the back or the front of head, inflammatory headaches slowly evolve over the entire head.
We have known for a long time that the brain itself does not have pain receptors and therefore can be the direct source of pain. But recent studies indicate there are pain fibers lining the inside of the blood vessels that course through the brain.
These pain fibers can be activated with the increased levels of pro-inflammatory cytokines that accompany chronic inflammatory conditions such as autoimmune disorders, intestinal bacterial overgrowth, dietary omega-3:6 fatty acid imbalances, reversible damage to the parasympathetic branch of the Autonomic Nervous System, tobacco smoke exposure, and chronic infections (hepatitis, HIV, etc.).
Interestingly, excessive AGE consumption may also activate increased levels of pro-inflammatory cytokines and cause inflammatory headaches. AGE’s are unusual molecules formed in high heat cooking conditions and in commercially prepared foods. If someone’s headaches are better or worse with changes in their diet they may be connected to not just what the person eats, but also connected to how the person’s food is prepared.
Unknown Patterns
And finally, some headaches fall into a category I call unknown because the chronic headache patterns do not fit in the above three groups. I suspect these headaches are usually caused by some combination of those other groups, but there are just no discernible patterns to them.
When presented with a patient with unknown headaches, I look for other symptoms the patient may have that are attributable to low brain blood pressure, sinus issues such as allergies or asthma, or inflammatory conditions. Treating these other issues often results in the unknown headaches resolving.
When people suffer from frequent headaches I ask them questions about their symptoms. I have found that when a patient is aware of these four headache locations and time of day patterns, their observations help lead us to the underlying problem.
I am an internal medicine physician (D.O.) from UCLA and my Internal Medicine and Autonomic practice is in the Phoenix area. I have discovered a multifaceted formula for Autonomic Nervous System restoration that is so groundbreaking that I was granted a patent for The Nemechek Protocol for Autonomic Recovery (Patent No. 10,335,396) in July 2019. For additional information, call my office 623-208-4226 or go to AutonomicMed.com.
This post is provided as an information resource only, and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be patient education, and does not create any patient-physician relationship.
© 2017. Dr. Patrick M. Nemechek and Jean R. Nemechek. All Rights Reserved.
My 10 yo had surgery to remove a large cholesteatoma from his middle ear in Nov 2018. (21 stitches behind his ear). Since then, he suffers from headaches at night, which seem to have suddenly worsened in the past month. They start after he lies down, and I usually have to give ibuprofen in the night. He says he feels like he is floating before the headaches start. The only thing the surgeon’s office recommends is Topamax (which i have not given) for migraine prevention. He has been on the protocol for 2 months. Might this be the inflammatory type… Read more »
Headaches that often worsen when lying down are most likely from sinus congestion/pressure issues.
Look at ways to improve decongestion.
Hi Dr. Nemecheck,
I read an research article on tVNS in the Journal of Headache and Pain and they recommended modulating the duty cycle 30 seconds on and 30 seconds off to avoid habituation. In your opinion is this necessary and if so, is the modulation setting in a standard TENS unit is sufficient to do this. Thanks again for your life changing amazing work.
The characteristics of VNS depend on the goals needing to be achieved.
Pain management, inflammatory control, epilepsy, depression/PTSD, neuroplasticity all require different current characteristics.
Most TENS units are not able to replicate these.
Hi Dr. Nemechek, I forgot to mention yesterday that I cannot try the Blood Pressure protocol (i.e. chicken broth) because I suffer from hypertension and I take 8mg of Coversyl and 30mg Nifedipine to lower it. So basically I’m scared to try it because of what it could do to my BP. However my BP is about 88/122 on average on my Rx, should I still try the chicken broth anyways while I keep taking my BP Rx?
I’m sorry but I can’t give you such specific advice.
Thank-you very much Dr. Nemechek, I will most definitely looking out for your new book in 2 months and adapt myself to the new appropriate dosage. Thanks again for responding to my question. Much appreciate it!
Hello Dr. Nemechek, I suffer from right temporal migraines, which are triggered by stress and certain foods. I started taking 1 1/2tsp of Inulin, 1 TBS Olive Oil and 600mg EPA and 300mg DHA for about 2 months now and I’ve been taking this in the morning and right after supper. Furthermore, I drink lots of water and I still get a lot of migraines. I don’t find I have much MORE of a bowl movements since I have been taking the combination of 3 ingredients. Do you have any suggestions of what I should be doing differently?
Your regimen is much more appropriate in dosage for an 8-year-old child with autism than an adult.
Our book discussing The Nemechek Protocol and how I deal with migraine headaches will not be released for another 2 months unfortunately.