Whether you have heartburn (GERD), bloating with meals, or symptoms commonly attributed to hypoglycemia, one of the most common causes for all of these conditions is a gastrointestinal disorder known as gastroparesis.
Gastroparesis is a Latin term for ‘paralyzed stomach’ and is used to describe various symptoms attributable to slow emptying of the stomach. Gastroparesis can lead to symptoms such as heartburn and GERD (gastroesophageal reflux disease) because when the normal and persistent production of stomach acid continues throughout the day without being emptied, stomach acid builds up and refluxes or splashes back up into the esophagus, causing the symptoms we commonly describe as heartburn or reflux.
Watch Dr. N’s CoffeeTalk on Heartburn
Sometimes the excessive collection of acid in the stomach will cause people to misinterpret the symptoms as low blood sugar or ‘hypoglycemia.’ This is because the excess stomach acid will make the person feel shaky, weak, hungry, and even nauseated, and when the person eats some food, the symptoms resolve. The association of these symptoms and their resolution with food is understandably but mistakenly attributed to low blood sugar.
The excessive stomach acid is actually causing the patient to experience low-grade nausea. Symptoms resolve because food stimulates the stomach to increase its emptying action and acts as an excellent acid neutralizer. We have experienced this before when we have been nauseated or vomiting from the flu or during pregnancy – we will eat some toast, soup, or crackers to help us deal with the nausea we experience.
The other important fact is that our physiology is designed to help us maintain normal blood sugar levels even if we go without food for extended periods. We were designed as Stone Age humans who were constantly exposed to unstable food supplies for millions of years and would often go for extended periods without eating. If we were to find ourselves in unfortunate circumstances where we went without food for weeks at a time, we might feel very hungry, but our blood sugar levels would remain constant for many weeks without food.
Other Symptoms Associated with Slow Stomach Motility
When the stomach’s grinding and emptying motility action is impaired, other portions of the intestinal tract may also be impaired. Under normal conditions, the stomach constantly empties its contents into the small intestine. From the upper esophagus all the way through to the colon, the intestinal tract operates like one long conveyor belt, with one portion of the GI tract passing its contents along to the next portion.
Sometimes patients will experience food (especially when it involves liquids) seeming to stick in the esophagus shortly after ingestion. They will feel a fullness or pressure in the chest, often below the breastbone (sternum).
They also experience some slowing of intestinal contents in the colon, resulting in constipation.
The slowed motility may also result in occasional frequent loose stools because of the overgrowth of colonic bacteria within the small intestine and the colon. A mixture of upwards of 500 different species of bacteria normally live within our intestinal tract. When the motility of the intestine slows down, a portion of the bacteria grows out of proportion to the others, resulting in diarrhea or urgency to have a bowel movement shortly after eating.
Autonomic Dysfunction is the Underlying Cause of Gastroparesis
I am convinced that most patients with heartburn or misinterpreted sense of hunger or low blood sugar have decreased intestinal motility because of underlying autonomic nervous system (ANS) abnormalities. The ANS is responsible for operating and coordinating the function of the body’s organs, such as the lungs, intestinal tract, cardiovascular system (heart, arteries, veins), and bladder.
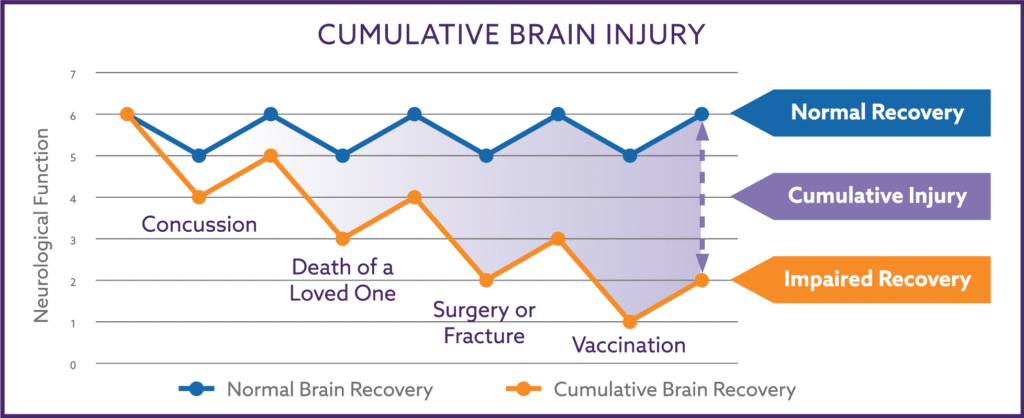
Dysfunction of the ANS can cause the slowing of intestinal tract motility and cause the bloating, heartburn, or constipation discussed above. The most common causes for autonomic dysfunction can be Insulin Resistance from obesity or excessive carbohydrate intake, a physically stressful event such as surgery, pregnancy, or a major illness. Some patients have a history of early childhood bloating, constipation, or heartburn.
Fortunately, most autonomic dysfunction can be accurately diagnosed and reversed with the elements of The Nemechek Protocol (high dose DHA, olive oil, balancing SIBO with rifaximin, and the use of vagus nerve stimulation).